The prevalence of anterior cruciate ligament (ACL) injuries among athletes and the general population has underscored the critical need for precise diagnostic techniques. In the realm of sports medicine and orthopedics, the Lachman test stands out as a fundamental evaluation method for detecting ACL integrity. This test, renowned for its simplicity and effectiveness, offers clinicians a direct approach to ascertain the extent of injury to one of the knee’s most crucial ligaments.
I. Technique
- Position the patient lying on their back (supine) and adjust their knee to a 20-30 degree angle of flexion. This positioning can be accomplished by placing a towel under the knee or the therapist positioning their own knee beneath the patient’s knee while on the bed.
- As recommended in Bates’ Guide to Physical Examination, the patient’s leg should also be gently turned outward (externally rotated). The examiner is to place one hand at the back of the tibia and the other on the patient’s thigh, ensuring the thumb is positioned on the tibial tuberosity.
- By pulling the tibia forward, a healthy ACL will restrict the tibia from moving forward on the femur, indicating a “firm end-feel.”
The Lachman test, unlike more complex diagnostic tools, requires minimal equipment and can be performed quickly in a clinical setting, making it an indispensable first step in the assessment of suspected ACL injuries. Its principal advantage lies in its ability to provide immediate insights into the ligament’s status, guiding further diagnostic and therapeutic decisions.
Despite advancements in imaging technologies like MRI, the Lachman test’s relevance remains undiminished. Its ability to deliver rapid results without the need for sophisticated machinery or extensive patient preparation ensures its continued prominence in orthopedic diagnostics. Moreover, the test’s high sensitivity and specificity have been consistently validated across numerous studies, affirming its accuracy and reliability in clinical practice.
However, the evolution of diagnostic methodologies has introduced arthrometers, such as the DYNEELAX® and GNRB®, as complementary tools that enhance the diagnostic landscape. These instruments, while not replacing the fundamental role of the Lachman test, offer quantifiable data on knee laxity and stability, providing a more nuanced understanding of the injury’s nature. This article aims to delve into the enduring significance of the Lachman test, exploring its unmatched value in ACL injury diagnostics, while also acknowledging how innovations like the DYNEELAX® and GNRB® arthrometers contribute to a more comprehensive assessment of knee ligament injuries.
In the following sections, we will explore the technique and interpretation of the Lachman test, review the evidence supporting its use by mentioning relevant & recent scientific publications, and discuss how arthrometers can be integrated into clinical practice to supplement the insights gained from this time-honored test.
II. The Anatomy of the ACL and Its Importance
Understanding the anatomy of the knee is pivotal in recognizing the significance of the anterior cruciate ligament (ACL), a key structure that ensures the stability and proper functioning of the knee joint. The knee, one of the body’s largest and most complex joints, integrates the femur (thigh bone), tibia (shin bone), and patella (kneecap) in a network of ligaments, tendons, and cartilage. Within this intricate assembly, the ACL plays a crucial role, extending from the posterior femur to the anterior tibia, and acts as a stabilizing force, preventing excessive forward movement of the tibia in relation to the femur.
The ACL’s primary function is to maintain knee stability during dynamic movements, such as pivoting, jumping, or sudden stops, which are common in various sports and physical activities. By limiting the anterior translation and rotation of the tibia, the ACL facilitates a range of motion essential for executing complex movements while safeguarding the knee from injury.
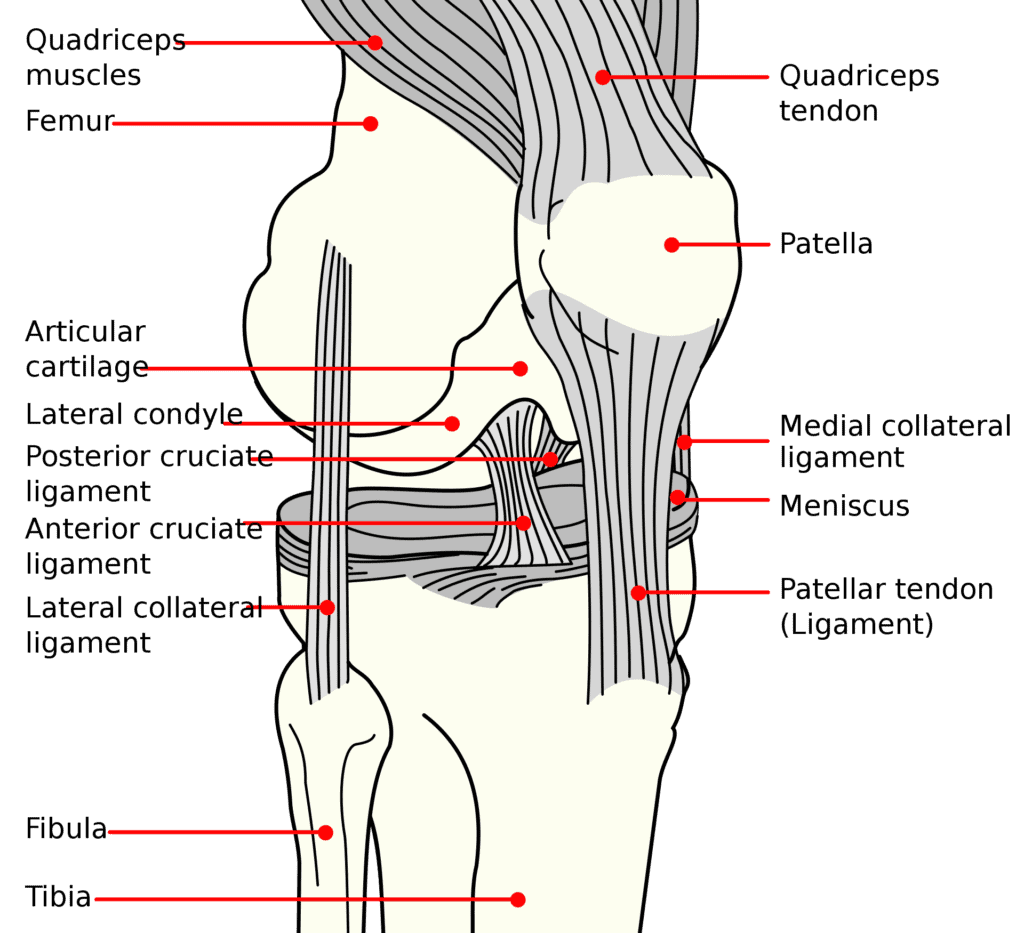
However, the ACL’s critical position and role render it susceptible to injuries, particularly through non-contact mechanisms like abrupt direction changes, awkward landings, or direct impacts from the front or side. Such injuries can range from partial tears, where the ligament is stretched but still functional, to complete tears, where the ligament fibers are fully severed.
The consequences of an ACL injury are profound, affecting not just the mechanical stability of the knee but also potentially leading to long-term issues such as meniscal tears and articular cartilage damage. The loss of ACL integrity compromises the knee’s structural balance, increasing the risk of secondary injuries and degenerative changes, including osteoarthritis. Beyond the physical ramifications, ACL injuries can significantly impact an individual’s quality of life, often necessitating prolonged periods of rehabilitation or surgical intervention to restore knee function.
Given the ACL’s vital role in knee stability and the severe implications of its injury, accurate and prompt diagnosis becomes paramount. This underscores the importance of the Lachman test, a diagnostic maneuver specifically designed to assess the integrity of the ACL by evaluating its ability to restrain anterior tibial translation. Understanding the anatomy and function of the ACL not only illuminates why the Lachman test is a cornerstone of clinical assessment but also highlights the necessity of comprehensive strategies for injury prevention, timely diagnosis, and effective treatment to preserve knee health and function.
III. The Lachman Test: Description and Interpretation

The Lachman test is a cornerstone diagnostic tool for assessing anterior cruciate ligament (ACL) integrity, crucial for maintaining knee stability and function. This segment elaborates on the technique and interpretation of the Lachman test, underpinned by scientific research, highlighting its indispensable role in clinical diagnostics for ACL injuries.
3.1 Description
The Lachman test is performed with the patient lying supine, where the knee is slightly flexed at an angle of approximately 20° to 30°. The examiner stabilizes the thigh while the other hand is placed on the back of the lower leg. A gentle but firm anterior force is applied to assess the forward movement of the tibia in relation to the femur. The feel at the endpoint, whether firm or “mushy,” is crucial for assessment. A “mushy” or indefinite endpoint typically indicates a compromised ACL.
3.2 Interpretation
Positive Result: An increased anterior movement of the tibia without a definitive endpoint suggests a potential ACL rupture. Negative Result: Minimal anterior translation with a solid endpoint suggests the ACL is intact.
3.3 Diagnostic Value
The Lachman test is highly valued for its sensitivity and specificity in detecting ACL injuries. Research underscores its superiority in sensitivity compared to other physical examinations like the anterior drawer and pivot shift tests.
One study by Sokal et al. in 2022, as detailed on PubMed, discusses the diagnostic accuracy of clinical tests for ACL tears, highlighting the comparative effectiveness of the Lachman test. This systematic review and meta-analysis pointed out that while the Lachman test has been previously overestimated, it remains comparably accurate for diagnosing ACL tears, especially in the absence of concomitant knee ligament injuries. It also highlighted the Lachman test’s effectiveness compared to other tests. This study noted that the pivot shift and Lever sign tests are most useful for diagnosing ACL injuries, but also emphasized that the Lachman test, particularly for complete tears and post-acute injuries, had a sensitivity of 68%-70% and a specificity of 79%-77%, which indicates its utility though slightly less than previously estimated (1).
Another investigation by Mulligan et al. in 2011 focused on the reliability and diagnostic accuracy of the Lachman test performed in a prone position, revealing high agreement between examiners and confirming its utility in diagnosing ACL tears. This research specifically examining the Lachman test in a prone position reported a 70% sensitivity and a 97% specificity, underlining the test’s reliability. Despite these promising figures, it advised against using the Lachman test as the sole diagnostic criterion (2).
Moreover, a systematic review by Huang et al. in 2016 and meta-analysis aimed to evaluate the sensitivity and specificity of three tests for assessing ACL ruptures, including the Lachman test. This study highlighted the Lachman test as the most sensitive method for determining ACL tears, showcasing its pivotal role in the diagnostic process (3).
An exploration within a broader diagnostic context reaffirmed the Lachman test as the most sensitive and specific method for diagnosing acute ACL tears, superior to both the anterior drawer test and the pivot shift test (Leblanc et al. 2015)(4).
The Lachman test is a fundamental element in the clinical assessment of ACL integrity. Its direct approach, coupled with high diagnostic accuracy and minimal discomfort to patients, solidifies its importance in orthopedic diagnostics and ACL injury management, supported by a wealth of empirical evidence.
Despite its proven diagnostic value, challenges remain. Decreased sensitivity for partial ruptures and the nuanced interpretation required for awake patients highlight areas for further research. These insights underscore the necessity of incorporating the Lachman test into a comprehensive diagnostic strategy, tailored to individual patient presentations and augmented by additional tests and imaging as needed.
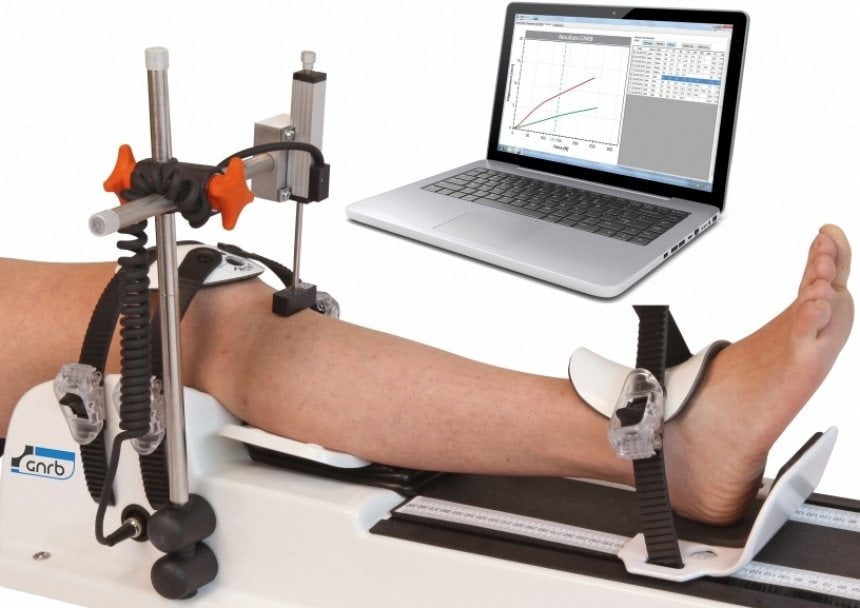
While the Lachman test has been established as a highly sensitive and specific method for diagnosing ACL injuries, advancements in medical technology have introduced innovative tools that complement traditional diagnostic techniques. Among these, robotic arthrometers, such as the DYNEELAX® and GNRB®, represent a leap forward in the precision and objectivity of knee ligament assessments. These devices offer quantifiable data on knee laxity and stability, providing a detailed analysis that supports the clinical findings obtained through manual tests. As we transition from the manual prowess of the Lachman test to the technological sophistication of robotic arthrometers, it’s crucial to explore how these advanced tools can enhance our diagnostic capabilities, offering a more comprehensive understanding of knee injuries and potentially guiding more personalized treatment strategies.
IV. Automated Lachman Test with Robotic Arthrometers: Dyneelax and GNRB
In the realm of orthopedic diagnostics, particularly in the assessment of knee ligament injuries, arthrometers like DYNEELAX® and GNRB® represent significant advancements in technology. These devices offer a quantitative approach to evaluating knee stability, providing clinicians with objective data to support their diagnoses. This section explores how these arthrometers function, their roles in diagnosing knee ligament injuries, and how they serve as complementary tools to traditional physical examinations like the Lachman test.

Arthrometers are sophisticated diagnostic tools designed to measure knee joint laxity and integrity with precision. The DYNEELAX® and GNRB® are among the forefront of these innovations, each with unique features tailored to enhance clinical assessments of knee ligament injuries.
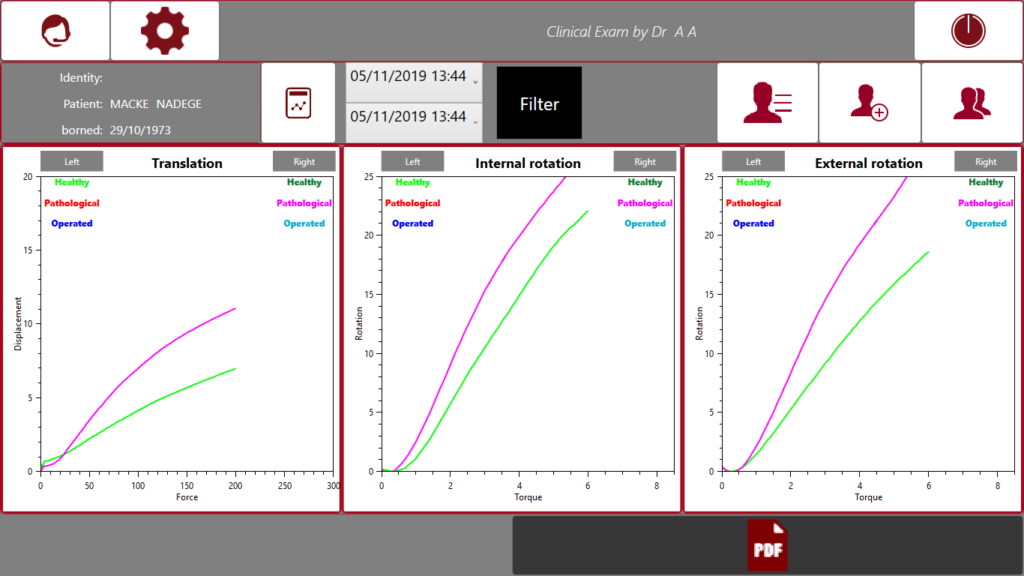
4.1 How Dyneelax and GNRB Work
The DYNEELAX® system represents a significant advancement in arthrometry, uniquely engineered to assess both the antero-posterior translation and medio-lateral rotation of the tibia relative to the femur. This capability to measure dual aspects of knee movement allows for an exhaustive evaluation of knee laxity, which is paramount for diagnosing ACL injuries. By quantifying both translational and rotational movements, DYNEELAX® offers a comprehensive view of knee stability, ensuring reproducible and accurate assessments that are critical for both initial diagnosis and monitoring rehabilitation progress.
In contrast, the GNRB® arthrometer specializes in automating the Lachman test, focusing on providing an objective measurement of anterior tibial translation under specified forces. It employs a sensor-equipped pad to exert force on the knee, capturing the tibia’s anterior movement. This data is instrumental in diagnosing both complete and partial ACL tears by delivering precise measurements of anterior knee laxity, albeit without assessing rotational stability.
Both DYNEELAX® and GNRB® stand as innovative tools in the orthopedic diagnostic landscape, offering advanced capabilities to measure knee ligament integrity. DYNEELAX®, with its dual-measurement feature, provides a broader assessment by measuring both translation and rotation, offering a more holistic view of knee stability. Meanwhile, GNRB® focuses on quantifying anterior tibial translation, closely mirroring the traditional Lachman test’s objectives. Together, these devices enhance the diagnostic process, offering objective, quantifiable data that complements the subjective assessments of physical examinations. Their integration into clinical practice underscores a commitment to precision and accuracy in diagnosing knee ligament injuries, ensuring patients receive the most informed and effective care possible.
4.1.1 Role in Diagnosing Knee Ligament Injuries
The primary role of arthrometers like DYNEELAX® and GNRB® is to provide an objective assessment of knee stability. In the context of ACL injuries, these devices offer detailed insights into the extent of ligament damage, which can be pivotal for determining the most appropriate treatment plan. By quantifying knee laxity, arthrometers help clinicians make informed decisions regarding the necessity of surgery, the potential for conservative management, and the prognosis for recovery.
Nowadays, various studies collectively affirm the GNRB® and DYNEELAX® arthrometers’ efficacy in ACL diagnostics. Kayla Smith et al. (5) validated GNRB®’s reliability in measuring ACL laxity with high intraclass correlation. Magdic et al. (6) highlighted its good intra-rater reliability. Théo Cojean compared GNRB® against MRI, showcasing its superior accuracy when diagnosing partial ACL tears (7).
Another study by Cojean (8) on DYNEELAX® demonstrated its potential in measuring both tibial translation and rotation, underscoring its diagnostic precision. These devices are valuable for objective ACL assessment, complementing traditional tests like the Lachman test.
The study by Seung Min Ryu et al. in 2018compared the diagnostic accuracy of the GNRB, Lachman test, and Telos device in acute ACL injuries. It concluded that the GNRB demonstrated superior diagnostic values over the Lachman test and Telos device, especially when evaluating injuries within 10 days of occurrence. This study highlights the GNRB as a highly effective and reliable tool for the early diagnosis of ACL injuries, outperforming traditional methods in both accuracy and reliability for acute cases.
4.1.2 Role in Monitoring Knee Ligaments After Reconstruction Surgery
The utilization of arthrometers in monitoring ACL grafts post-reconstruction extends their application from initial diagnosis to comprehensive post-surgery care. Highlighted by research from Pouderoux (10), Semay (11), Nouveau (12), and Forelli (13), these tools provide clinicians with objective metrics on graft healing and knee stability over time. This data is pivotal for customizing rehabilitation protocols, ensuring a balance between recovery and the prevention of re-injury. Through such detailed monitoring, arthrometers facilitate a deeper understanding of graft integration processes, significantly contributing to the advancement of post-operative ACL care strategies.
4.2 Complementing the Lachman Test
While the Lachman test is a gold standard for clinically assessing ACL integrity due to its high sensitivity and specificity, arthrometers like DYNEELAX® and GNRB® enhance the diagnostic process. They provide quantifiable data that complement the subjective findings from physical examinations. This objective information can be especially useful in cases where physical exam results are inconclusive or when evaluating the knee’s stability over time.
Furthermore, the use of arthrometers can standardize the assessment process, reducing variability between examiners and ensuring consistent measurements across different clinical settings. By integrating these tools into the diagnostic workflow, clinicians can achieve a more comprehensive understanding of knee injuries, leading to tailored and effective treatment strategies.
Arthrometers such as Dyneelax and GNRB represent a significant advancement in the field of orthopedics, offering clinicians a precise and objective method for assessing knee ligament injuries. While these devices do not replace the need for clinical examination skills, such as those employed in the Lachman test, they significantly enhance the accuracy and reliability of diagnoses. By providing objective measurements of knee laxity, arthrometers help bridge the gap between clinical assessment and imaging studies, ultimately improving patient outcomes through more informed treatment decisions. As technology evolves, the integration of such devices into routine clinical practice will undoubtedly continue to transform the landscape of orthopedic diagnostics, ensuring that patients receive the most accurate diagnoses and effective treatments possible.
4.3 Dynamic Asssessments + Static MRI Assessments.
Integrating arthrometers such as DYNEELAX® and GNRB® into clinical practice, alongside traditional assessments like the Lachman test, significantly enhances the diagnostic process for ACL injuries. These devices offer a dynamic and quantitative analysis of knee stability, providing a complementary tool to MRI by elevating patient treatment plans through precise measurements of both antero-posterior translation and medio-lateral rotation.
The Dyneelax system’s unique capability to assess knee rotation is particularly valuable, as it can indicate the necessity for extra-articular procedures such as lateral extra-articular tenodesis (LET) or Lemaire techniques. This advanced diagnostic insight ensures a comprehensive approach to ACL injury treatment, addressing both the intra and extra-articular components of knee instability.
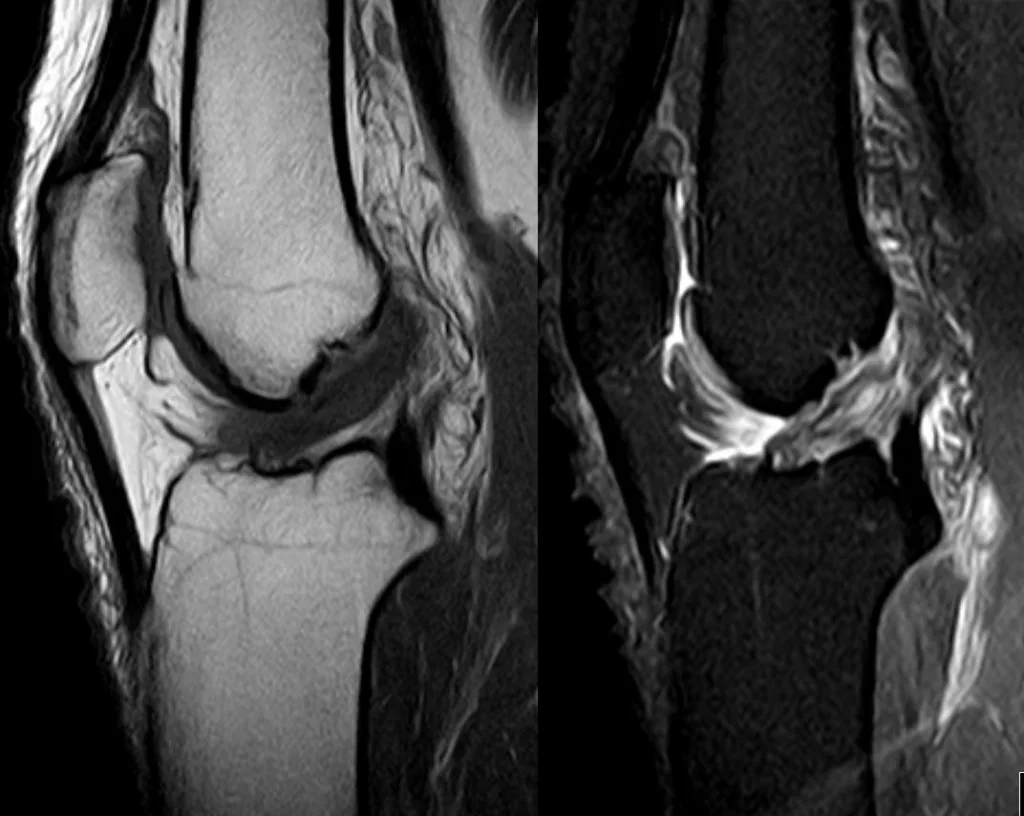
Moreover, the use of arthrometers aims to complement, not replace, MRI. By employing DYNEELAX® and GNRB® for initial assessments, clinicians can make informed decisions about which patients truly require MRI, thereby optimizing the use of imaging resources. This strategy not only enhances diagnostic accuracy, especially in cases of partial ACL ruptures as stipulated by Cojean et al. in 2023 (7), but also contributes to making room in MRI schedules for patients with other pathologies.
Incorporating arthrometers into the diagnostic workflow allows for a more efficient allocation of healthcare resources. By identifying patients who need further evaluation with MRI, and those whose treatment plans can be determined based on the arthrometer’s findings, clinicians can ensure timely and appropriate care. This approach underscores the importance of dynamic assessment in ACL injury diagnosis and the role of technology in streamlining patient management.
In essence, the integration of Dyneelax and GNRB into clinical evaluations represents a modern approach to diagnosing knee ligament injuries, leveraging technology to provide targeted and effective treatments. This not only elevates the standard of care but also enhances the efficiency and effectiveness of healthcare delivery in the realm of orthopedic diagnostics.
4.4 Scenarios Where Arthrometers Provide Additional Value
Complex Diagnoses: In cases where patients present with multi-directional knee instability, Dyneelax’s capacity to assess both translation and rotation offers critical insights that can guide more targeted treatment plans.
Post-operative Assessment: Following ACL reconstruction, both DYNEELAX® and GNRB® can objectively monitor healing progress and knee stability, informing rehabilitation protocols and the timing of return to activity.
Research and Longitudinal Studies: These tools are invaluable in research settings for establishing baseline knee laxity measures in athletes or in longitudinal studies tracking the natural history of ACL injuries and outcomes post-intervention.
Pediatric Patients: In younger patients where growth plates must be considered, and clinical examinations might be challenging due to patient cooperation, arthrometers provide objective, reproducible assessments that can aid in the decision-making process for conservative versus surgical management.
Integrating arthrometers into clinical practice not only augments the diagnostic accuracy for ACL injuries but also enriches patient care by enabling precise monitoring and evidence-based decision-making. While traditional physical examination techniques remain fundamental, the addition of DYNEELAX® and GNRB® arthrometers offers a modern approach that leverages technology for improved outcomes.
Conclusion
The Lachman test remains the cornerstone in the diagnosis of anterior cruciate ligament (ACL) injuries, exemplifying its crucial role amidst the advancements in medical diagnostics. This enduring relevance highlights the essential nature of mastering the Lachman test for clinicians, emphasizing its unparalleled sensitivity and specificity in evaluating the ACL’s integrity.

While arthrometers such as DYNEELAX® and GNRB® have introduced sophisticated quantitative assessments, enriching the landscape of diagnostic tools available, they serve to complement rather than replace the foundational clinical examination techniques. These devices offer valuable data on knee laxity, but the nuanced, skillful application of the Lachman test by a trained clinician remains paramount. It is this blend of traditional expertise and technological innovation that marks a significant stride in enhancing patient care.
The call for continued research and training in this area is loud and clear. Advancements in diagnostic accuracy and the integration of innovative technologies like arthrometers into routine clinical practice promise to refine our approach to ACL injury diagnosis further. Such endeavors not only aim to improve patient outcomes but also contribute significantly to the field of sports medicine and orthopedics at large.
Enhancing the accuracy of ACL diagnostics through ongoing education and embracing new technologies reflects our commitment to providing the highest standard of care. As we forge ahead, the integration of empirical evidence, clinical expertise, and cutting-edge tools will ensure that our diagnostic capabilities continue to evolve, offering patients the most informed and effective treatment options available.
In essence, the journey from the Lachman test to the use of advanced arthrometers encapsulates the dynamic nature of medical practice—where tradition meets innovation. It’s a testament to the medical community’s dedication to excellence in patient care, underscoring the importance of both preserving the invaluable clinical skills passed down through generations and embracing the future of medical diagnostics.
Medical References (Link in DOI)
- Sokal, P. A., Norris, R., Maddox, T. W., & Oldershaw, R. A. (2022). The diagnostic accuracy of clinical tests for anterior cruciate ligament tears are comparable but the Lachman test has been previously overestimated: a systematic review and meta-analysis. Knee Surgery, Sports Traumatology, Arthroscopy, 30(10), 3287-3303. DOI: 10.1007/s00167-022-06898-4
- Mulligan, E. P., Harwell, J. L., & Robertson, W. J. (2011). Reliability and diagnostic accuracy of the Lachman test performed in a prone position. Journal of Orthopaedic & Sports Physical Therapy, 41(10), 749-757. DOI: 10.2519/jospt.2011.3761
- Huang, W., Zhang, Y., Yao, Z., & Ma, L. (2016). Clinical examination of anterior cruciate ligament rupture: a systematic review and meta-analysis. Acta Orthopaedica et Traumatologica Turcica, 50(1), 22-31. DOI: 10.3944/AOTT.2016.14.0283
- Leblanc, M.-C., Kowalczuk, M., Andruszkiewicz, N., Simunovic, N., Farrokhyar, F., Turnbull, T. L., Debski, R. E., & Ayeni, O. R. (2015). Diagnostic accuracy of physical examination for anterior knee instability: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy, 23(10), 2805-2813. DOI: 10.1007/s00167-015-3563-2
- Smith K, Miller N, Laslovich S. (2022). The Reliability of the GNRB® Knee Arthrometer in Measuring ACL Stiffness and Laxity: Implications for Clinical Use and Clinical Trial Design. Int J Sports Phys Ther, 17(6), 1016-1025. DOI: 10.26603/001c.38252
- Magdić M, Gošnak Dahmane R, Vauhnik R. (2023). Intra-rater reliability of the knee arthrometer GNRB® for measuring knee anterior laxity in healthy active subjects. Journal of Orthopaedics. DOI: 10.1016/j.jor.2023.03.016
- Cojean T, Batailler C, Robert H, Cheze L. (2023). GNRB® laximeter with magnetic resonance imaging in clinical practice for complete and partial anterior cruciate ligament tears detection: A prospective diagnostic study with arthroscopic validation on 214 patients. Knee, 42, 373-381. DOI: 10.1016/j.knee.2023.03.017
- Cojean, T., Batailler, C., Robert, H., Cheze, L. (2023). Sensitivity repeatability and reproducibility study with a leg prototype of a recently developed knee arthrometer: The DYNEELAX®. Medicine in Novel Technology and Devices, 19, 100254. DOI: 10.1016/j.medntd.2023.100254
- Ryu, S. M., Na, H. D., & Shon, O. J. (2018). Diagnostic Tools for Acute Anterior Cruciate Ligament Injury: GNRB, Lachman Test, and Telos. Knee Surgery & Related Research, 30(2), 121-127. DOI: 10.5792/ksrr.17.014
- Pouderoux, T., Muller, B., Robert, H. (2019). Joint laxity and graft compliance increase during the first year following ACL reconstruction with short hamstring tendon grafts.. DOI: 10.1007/s00167-019-05711-z
- Semay, B., Rambaud, A., Philippot, R., Edouard, P. (2016). Evolution of the anteroposterior laxity by GnRB at 6 9 and 12 months post-surgical anterior cruciate ligament reconstruction. DOI: 10.1016/j.rehab.2016.07.045
- Nouveau, S., Robert, H., Viel, T. (2017). ACL Grafts Compliance During Time: Influence of Early Solicitations on the Final Stiffness of the Graft after Surgery. Journal of Orthopedic Research and Physiotherapy, 3(1), 035. DOI: 10.24966/ORP-2052/100035
- Forelli F, Le Coroller N, Gaspar M, et al. (2023). Ecological and Specific Evidence-Based Safe Return To Play After Anterior Cruciate Ligament Reconstruction In Soccer Players: A New International Paradigm. IJSPT. Published online April 2, 2023. DOI: 10.26603/001c.73031