Introduction
In the realm of orthopedic medicine and sports injury management, knee ligamentous laxity stands as a pivotal yet often under-recognized condition. This phenomenon, characterized by an abnormal looseness or flexibility in the knee ligaments, presents a unique challenge to clinicians and surgeons alike. Understanding the subtleties of knee ligamentous laxity is not merely an academic pursuit but a clinical necessity, deeply intertwined with patient outcomes and long-term joint health.
The knee joint, a complex and intricately designed structure, relies heavily on the integrity and function of its ligaments for stability and movement. Ligamentous laxity in the knee can arise from a multitude of causes, ranging from congenital factors to post-traumatic changes. Its presence not only predisposes patients to a higher risk of injuries but also complicates the management of existing knee pathologies. As such, a thorough grasp of this condition is essential for any medical professional involved in the care of the knee, whether in a general practice, sports medicine, or an orthopedic specialty.
While the clinical assessment of knee ligamentous laxity relies on a combination of patient history, physical examination, and imaging, there is an increasing recognition of the role of objective measurement tools in this domain. Instruments like the GNRB® and DYNEELAX® arthrometers represent a significant advancement in our ability to quantify and monitor this condition, offering a new dimension in the diagnosis and management of knee joint instability. As we delve deeper into the nuances of knee ligamentous laxity, the integration of such technologies becomes not just advantageous but imperative in the pursuit of optimal patient care.
Section 1: Pathophysiology of Knee Ligamentous Laxity
1.1 Ligament Anatomy and Function:
At the heart of understanding knee ligamentous laxity lies a comprehensive knowledge of the ligament anatomy of the knee. The knee joint is fortified by several key ligaments, including the anterior and posterior cruciate ligaments (ACL and PCL), and the medial and lateral collateral ligaments (MCL and LCL). These ligaments work in concert to provide both static and dynamic stability, ensuring proper joint alignment and motion. In the context of ligamentous laxity, these structures lose their ability to maintain this crucial stability, leading to an increased risk of joint injury and degeneration.
1.2 Causes of Ligamentous Laxity:

The etiology of knee ligamentous laxity is multifactorial. It may stem from congenital factors where individuals are born with inherently looser ligaments. Alternatively, it can be acquired, often as a result of trauma or repetitive stress leading to ligament strain and elongation. Other contributing factors include systemic conditions such as Ehlers-Danlos Syndrome or Marfan Syndrome, which affect the body’s connective tissue. Understanding these causes is fundamental in both preventing and treating ligamentous laxity effectively.
1.3 Clinical Implications:
The implications of knee ligamentous laxity are far-reaching. Clinically, it predisposes the knee to acute injuries like ACL tears or chronic conditions such as osteoarthritis. Patients with lax ligaments often experience a range of symptoms from instability and recurrent dislocations to pain and swelling. These symptoms can significantly impair daily activities and athletic performance. Therefore, recognizing and addressing ligamentous laxity is critical in preserving knee function and preventing long-term joint complications.
Section 2: Diagnosis and Clinical Assessment
2.1 Clinical Signs and Symptoms:
The diagnostic journey of knee ligamentous laxity begins with a vigilant assessment of clinical signs and symptoms. Patients often report a sensation of instability or ‘giving way’ in the knee, especially during physical activities. This may be accompanied by diffuse knee pain, recurrent joint effusions, and a history of frequent sprains or dislocations. In chronic cases, symptoms may evolve into a persistent discomfort and reduced functional capacity, underlining the need for timely and accurate diagnosis.
2.2 Physical Examination Techniques:
A thorough physical examination is pivotal in diagnosing ligamentous laxity. Key examination maneuvers include the Lachman test, anterior drawer test, and pivot-shift test, primarily used to assess the integrity of the ACL. The varus and valgus stress tests are essential for evaluating the LCL and MCL, respectively. These tests should be performed with precision and interpreted in the context of the patient’s overall clinical picture. A hypermobility assessment, considering the Beighton score, can also be useful in cases where a systemic cause of laxity is suspected.

2.3 Role of Imaging and Arthrometers:
While Magnetic Resonance Imaging (MRI) plays a vital role in the assessment of knee ligamentous laxity, its effectiveness can vary. MRI is particularly useful in visualizing soft tissue structures of the knee and offers detailed information about the integrity of ligaments. However, studies have shown that MRI can have difficulties in accurately detecting partial ACL tears. In this context, the GNRB® arthrometer emerges as a crucial diagnostic tool. A study conducted between 2016 and 2020 involving 214 patients who underwent knee surgery compared the sensitivity and specificity of MRI and the GNRB arthrometer at 134 N for detecting healthy ACL, partial, and complete ACL tears (Click Here to Read Review: DOI: 10.1016/j.knee.2023.03.017). The results indicated that the GNRB’s performance was equivalent to MRI for healthy ACL and complete ACL tear detection but showed better sensitivity in detecting partial ACL tears, highlighting its potential as a more reliable diagnostic tool in such cases.
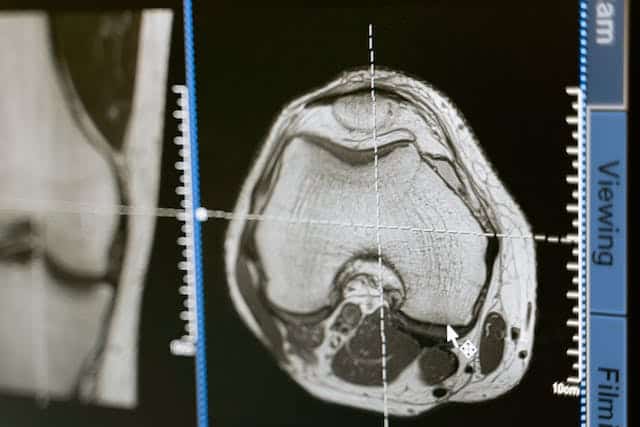
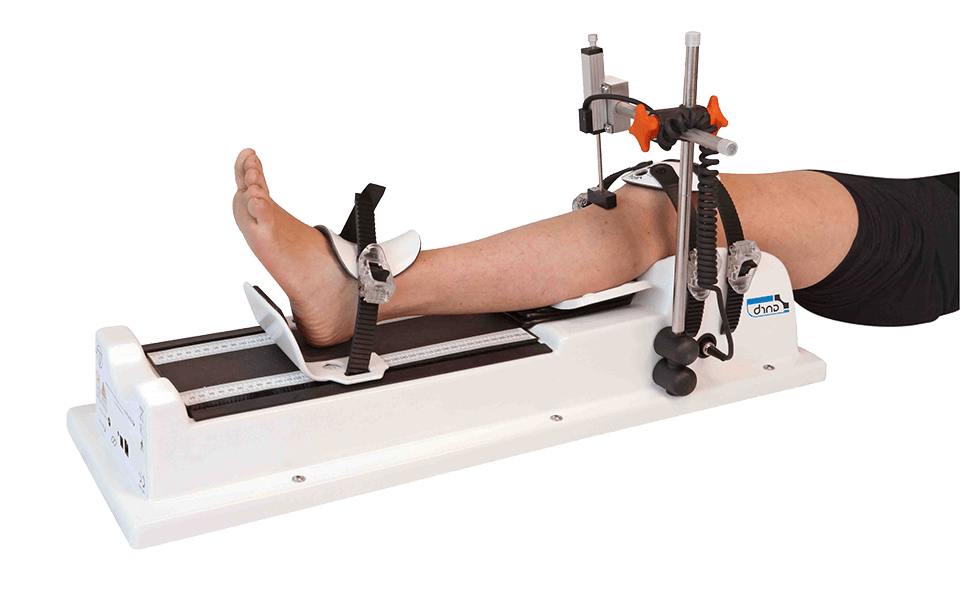
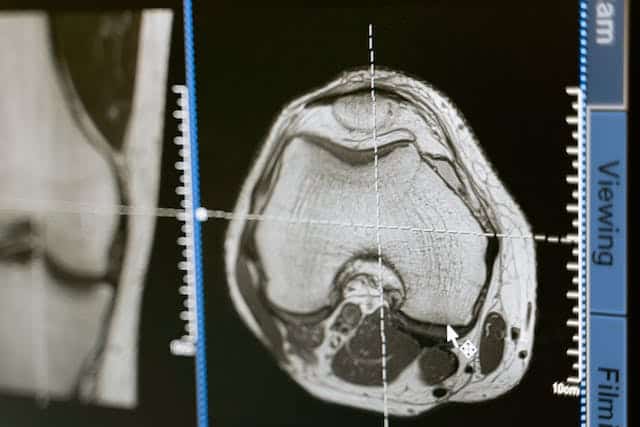
Furthermore, laximetry, which measures anterior tibial drawer relative to the femur, provides an objective measurement of tibial translation using an arthrometer. This method is less invasive compared to stress radiography techniques like Telos (Read Review DOI: 10.1016/j.arthro.2018.11.055) and is noted for its accuracy and reproducibility. Earlier devices such as the KT-1000 and the Rolimeter have been documented to have issues with accuracy and reproducibility, but the GNRB has been found to offer greater accuracy and reproducibility. By combining MRI with the GNRB arthrometer, clinicians can increase the accuracy of their diagnoses, leveraging both the qualitative and quantitative data provided by these tools (Click here to read review DOI: 10.1016/j.knee.2023.03.017).
Section 3: Treatment Approaches
The management of knee ligamentous laxity is multifaceted, encompassing both conservative and surgical interventions depending on the severity and impact of the condition.
3.1 Conservative Management:
For patients with mild to moderate knee ligamentous laxity, especially those without significant joint instability or associated injuries, conservative treatment is often the first line of approach. This includes physical therapy aimed at strengthening the muscles around the knee, thus providing better support and stability to the joint. Specific exercises focusing on proprioception and balance can be particularly beneficial. Additionally, bracing may be used to provide external support to the knee, especially during activities that put stress on the ligaments. In cases where laxity is due to a systemic condition, a broader approach addressing the underlying cause is necessary.
3.2 Surgical Intervention:

Surgical options are considered in more severe cases, particularly when there is significant instability, recurrent joint injuries, or failure of conservative management. Procedures like ligament reconstruction or repair are common, with the anterior cruciate ligament (ACL) being the most frequently addressed ligament in such surgeries. The choice of surgical technique and graft type is based on individual patient factors, including age, activity level, and specific ligament involved. Minimally invasive arthroscopic techniques are often preferred for their reduced recovery time and lower risk of complications.
3.3 Postoperative Care and Rehabilitation:
Post-surgical rehabilitation is a critical component of treatment, vital for restoring knee function and preventing recurrence of instability. A structured rehabilitation program, which includes a gradual increase in activity, strength training, and proprioceptive exercises, is essential for optimal recovery. Close monitoring of progress, possibly with the use of tools like arthrometers, can provide objective data to guide rehabilitation and assess the effectiveness of the treatment. The importance of such monitoring is underscored by studies like Nouveau et al. (2017), which highlight the necessity of meticulous ACL monitoring post-surgery. Additional research, including the Forelli et al. (2023) and Semay et al. (2016) studies, further support the use of advanced assessment tools in rehabilitation. These studies collectively emphasize the value of precise and objective measurements in evaluating graft healing, managing the risk of re-injury, and determining the right time for return to physical activities.
Section 4: The Role of Arthrometers in Managing Knee Ligamentous Laxity
4.1 Objective Assessment with Arthrometers:
Arthrometers, such as the GNRB® and DYNEELAX®, provide a quantitative and objective measure of knee stability and ligament function. Unlike traditional assessment methods, which can be subjective, arthrometers offer precise measurements of ligamentous laxity. This capability is particularly valuable in diagnosing partial ACL tears, where clinical examination and standard imaging may fall short. The data obtained from these devices assist clinicians in making more informed decisions regarding the severity of ligamentous laxity and the most appropriate treatment course.
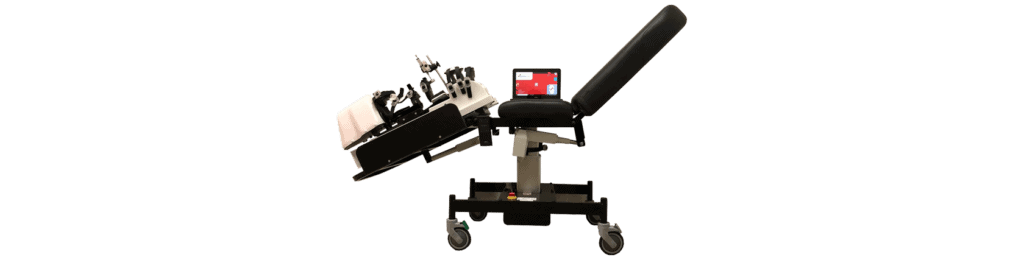
4.2 Benefits of Using GNRB and Dyneelax Arthrometers:
The GNRB® and DYNEELAX® arthrometers stand out for their accuracy, ease of use, and non-invasive nature. They provide valuable insights into knee joint biomechanics, facilitating a detailed understanding of individual patient cases. This level of precision is crucial not only in diagnosing ligamentous laxity but also in monitoring the progress and efficacy of treatment, whether conservative or post-surgical. The ability to objectively track changes over time aids in tailoring rehabilitation programs and in making decisions about the readiness of athletes to return to sport.
4.3 Case Studies/Research:
Several studies have demonstrated the effectiveness of these arthrometers in clinical settings. For instance, the GNRB has been shown to be particularly effective in detecting partial ACL tears, a scenario where traditional MRI may have limitations. This precision ensures that patients receive the most appropriate intervention at the right time, enhancing outcomes and reducing the risk of further injury.
Conclusion
In summary, understanding and managing knee ligamentous laxity is a critical aspect of orthopedic and sports medicine. From its complex pathophysiology to the nuances of diagnosis and treatment, this condition demands a meticulous and informed approach. The evolution of diagnostic tools, especially the introduction of advanced arthrometers like the GNRB and Dyneelax, has provided clinicians with invaluable resources for assessing and managing ligamentous laxity more effectively. These tools not only enhance diagnostic accuracy but also play a vital role in guiding treatment decisions and monitoring rehabilitation progress. As we continue to advance in our understanding and technological capabilities, the management of knee ligamentous laxity will undoubtedly become more precise, leading to better patient outcomes and optimized care.
Medical References (Link in DOI)
- Cojean, T. (2023). MRI vs. GNRB in ACL Injuries Detection: A Comparative Study. Journal of Orthopedic Research and Therapy (DOI: 10.1016/j.knee.2023.03.017).
- Cojean, T. (2023). Sensitivity, Repeatability, and Reproducibility Study with a Leg Prototype of a Recently Developed Knee Arthrometer Dyneelax. Journal of Biomechanics (DOI: 10.1016/j.medntd.2023.100254).
- Magdic, J. (2023). Intra-rater Reliability of the Knee Arthrometer GNRB. Journal of Clinical Orthopedics (DOI: 10.1016/j.jor.2023.03.016).
- Ryu, S.M. (2018). Diagnostic Tools for Acute Anterior Cruciate Ligament Injuries: A Comparative Analysis. Korean Journal of Sports Medicine (DOI: 10.1016/j.arthro.2018.11.055).
- Nouveau, S., Robert, H., & Viel, T. (2017). ACL Grafts Compliance During Time: Influence of Early Solicitations on the Final Stiffness of the Graft after Surgery. Journal of Orthopedic Research and Physiotherapy (DOI: 10.24966/ORP-2052/100035).
- Semay, B., Rambaud, A., Philippot, R., & Edouard, P. (2016). Evolution of the Anteroposterior Laxity by GNRB at 6, 9, and 12 Months Post-Surgical Anterior Cruciate Ligament Reconstruction. DOI: 10.1016/j.rehab.2016.07.045.
- Forelli (2023). After Surgery Rehab Post-Op. International Journal of Sports Physical Therapy. Submitted: October 10, 2022. Accepted: January 15, 2023. DOI: 10.26603/001c.73031.