Introduction
The Anterior Cruciate Ligament (ACL) is a cornerstone of knee stability and dynamic movement. As an integral part of the knee’s complex structure, the ACL is crucial for rotational stability and preventing the anterior displacement of the tibia relative to the femur. Its role is especially critical in sports and activities that involve sudden changes in direction, pivoting, or jumping.
However, the ACL is prone to injury, particularly among athletes and those leading active lifestyles. The frequency of ACL injuries presents a significant concern, with estimates suggesting around 400,000 ACL reconstructions each year in the United States (Martha M. Murray – 2021 – DOI: 10.1002/jor.25128). Sports such as soccer, basketball, and skiing, which demand quick and intense directional shifts, see a higher incidence of these injuries.
These injuries not only jeopardize athletic pursuits but also carry long-term risks for joint health, including the potential development of conditions like osteoarthritis. Thus, a comprehensive understanding of ACL injuries and their surgical treatment is crucial in sports medicine and orthopedic practice. This guide is designed to provide a detailed exploration of ACL surgery, covering everything from diagnosis to recovery for both patients and healthcare providers.
This article will answer questions like:
1. Anatomy and Function of the ACL
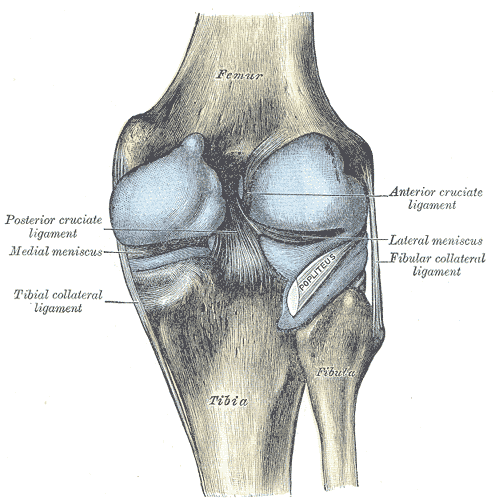
The Anterior Cruciate Ligament (ACL), an essential component within the knee joint, connects the femur (thigh bone) to the tibia (shin bone). This ligament, typically about 38mm in length and 10mm in width, plays a crucial role in maintaining the anterior-posterior stability of the knee. Its unique, crisscross configuration with the Posterior Cruciate Ligament (PCL) ensures a balanced and controlled range of motion.
Functionally, the ACL is vital in providing rotational stability, especially during dynamic activities. It serves as a key stabilizer in movements involving pivoting, lateral maneuvers, or sudden directional shifts. This is particularly important in sports with rapid accelerations, decelerations, and agile turns.
The pathophysiology of ACL injuries is intricately linked to its role. Injuries primarily occur through two mechanisms: acute trauma and athletic injuries. Acute trauma typically involves a direct impact to the knee, as seen in vehicular accidents or contact sports. Athletic injuries, on the other hand, are often non-contact, occurring during abrupt stops, jumps, or shifts in direction, which place abnormal stress on the ACL.
These mechanisms can lead to various injuries, ranging from partial tears to complete ruptures of the ACL. The severity of these injuries significantly affects knee mechanics. A compromised ACL leads to diminished knee stability, heightening the risk of further knee damage, including meniscal and cartilage injuries. Over time, this instability can contribute to the onset of osteoarthritis, characterized by the breakdown of cartilage and joint degeneration.
Understanding the ACL’s anatomy, function, and the mechanisms and pathophysiology of its injuries is critical for effective diagnosis, treatment, and prevention. This knowledge is foundational for surgical interventions and rehabilitation strategies aimed at restoring optimal knee function and health.
2. Indications for ACL Reconstruction Surgery
When deliberating ACL reconstruction, the decision to opt for surgery over conservative management involves a comprehensive assessment of multiple factors. This includes evaluating patient-specific criteria, discerning clinical indications, and acknowledging potential contraindications. The underlying determinant is often the individual’s activity level, ambitions for athletic participation, and the degree of knee instability experienced.
A crucial aspect of this decision-making process is the employment of preoperative imaging. Magnetic Resonance Imaging (MRI), a static test, provides a detailed assessment of the ACL’s integrity and identifies associated intra-articular pathologies like meniscal tears or cartilage damage. However, to complement the static insights from MRI, dynamic testing of the knee is increasingly recognized as essential in clinical evaluation.
Dynamic arthrometers, such as Dyneelax and GNRB, are instrumental in this regard. These devices simulate real-life stresses on the knee, mimicking the conditions under which most ACL injuries occur. By quantifying knee laxity under life-like conditions, these tools provide a more functional assessment of the ligament’s competency. This dynamic evaluation is particularly valuable in identifying partial ruptures of the ACL, which might be less apparent in static MRI scans (Read Study from Théo Cojean – 2023). The combination of MRI and dynamic arthrometry offers a more holistic understanding of the knee’s condition, enhancing the precision of the diagnosis and aiding in crafting a more tailored surgical plan.

Patient counseling remains a critical component in preoperative planning. This involves setting realistic expectations about the surgery, recovery timeline, potential outcomes, and discussing the rehabilitation process and associated risks. It’s crucial for patients to understand the likelihood of returning to pre-injury activity levels, ensuring that their decisions align with their personal, lifestyle, and occupational needs.
Specific scenarios often necessitate ACL reconstruction. Persistent knee instability, particularly episodes of ‘giving way’ in daily or sports activities, strongly suggests the need for surgery. For individuals in high-demand sports or occupations involving significant pivoting or jumping, ACL reconstruction is often recommended to restore joint stability and function. The presence of concomitant knee injuries, such as meniscal or cartilage damage, also frequently warrants surgical intervention.
The decision for surgery considers not just physical symptoms or radiological findings, but also factors like age, overall health, knee condition, and willingness to undergo rehabilitation. While younger, active individuals may benefit more from surgery, conservative management might be more suitable for older patients or those leading a sedentary lifestyle.
The impact of lifestyle and occupational demands plays a crucial role in this decision. Athletes, military personnel, or individuals with physically demanding jobs typically require a stable knee for optimal performance. In these cases, ACL reconstruction provides the best opportunity for a return to pre-injury activity levels. Conversely, those with minimal physical demands or the ability to modify activities to avoid high stress on the knee might consider non-surgical management.
In conclusion, the decision to proceed with ACL surgery is highly individualized, involving careful consideration of the patient’s specific situation, functional demands, knee stability, associated injuries, and overall health status. The ultimate goal is to tailor the treatment approach to optimize outcomes, ensuring a return to functional mobility and an active lifestyle.
As we embark on a detailed exploration of Section 3, it’s essential to appreciate the transformative journey ACL surgery has undergone. This section aims to unravel the sophisticated surgical techniques developed for ACL reconstruction, tracing the path from the early days of open surgery to the contemporary pinnacle of arthroscopic precision. We’ll explore the nuances of graft selection, the meticulous steps of the surgical procedure, and the innovations that continue to shape patient outcomes in the dynamic field of orthopedic medicine.
3. Optimal Timing for ACL Surgery - How soon should you get ACL surgery after your injury diagnosis?
In cases of a complete ACL rupture, the timing for reconstructive surgery is typically set between three to six weeks post-injury. This interval allows for the reduction of inflammation around the injury site. Early surgery can lead to excessive scarring, known as arthrofibrosis.

The decision on when to perform the surgery is influenced by several factors, as determined by orthopedic surgeons:
- Presence of additional injuries requiring prior treatment.
- The knee’s physical condition.
- The patient’s level of discomfort.
- The patient’s ability to move the knee, specifically the range and control in bending and straightening the leg.
Research indicates that postponing ACL reconstruction surgery beyond six months after the injury can diminish the likelihood of achieving a significant improvement. Additionally, this delay can increase the probability of requiring further ACL revision surgeries in the future.
This was put forward by a key 2021 study by Brian Forsythe et al. It was observed that patients who had their surgery after this period were less likely to achieve patient-acceptable symptomatic states (PASS) and had a higher likelihood of requiring revision ACL reconstruction. This implies that postponing surgery might lead to poorer outcomes and an increased chance of relapse.
4. Surgical Techniques for ACL Reconstruction - A Complete Overview
4.1 Historical Evolution of ACL Surgery
The progression of ACL surgery represents a significant chapter in orthopedic medicine. Initially, during the early 20th century, open surgical techniques were employed, involving larger incisions and direct visualization of the knee structures. These methods, while effective, resulted in considerable postoperative pain and lengthy recovery periods.
The 1970s marked a turning point with the introduction of arthroscopic techniques by Dr. Masaki Watanabe, which revolutionized ACL surgery. This minimally invasive approach, utilizing small incisions and a fiberoptic camera, allowed for enhanced visualization, reduced tissue trauma, and faster patient recovery. Over the years, continuous refinements in arthroscopic technology and surgical techniques have further improved the precision and outcomes of ACL reconstruction, making it one of the most successful procedures in sports medicine.
4.2 Reconstruction vs. Repair
In the treatment of ACL injuries, there are two main approaches: reconstruction and repair. Each method has distinct techniques and is suited for different types of injuries and patient needs.
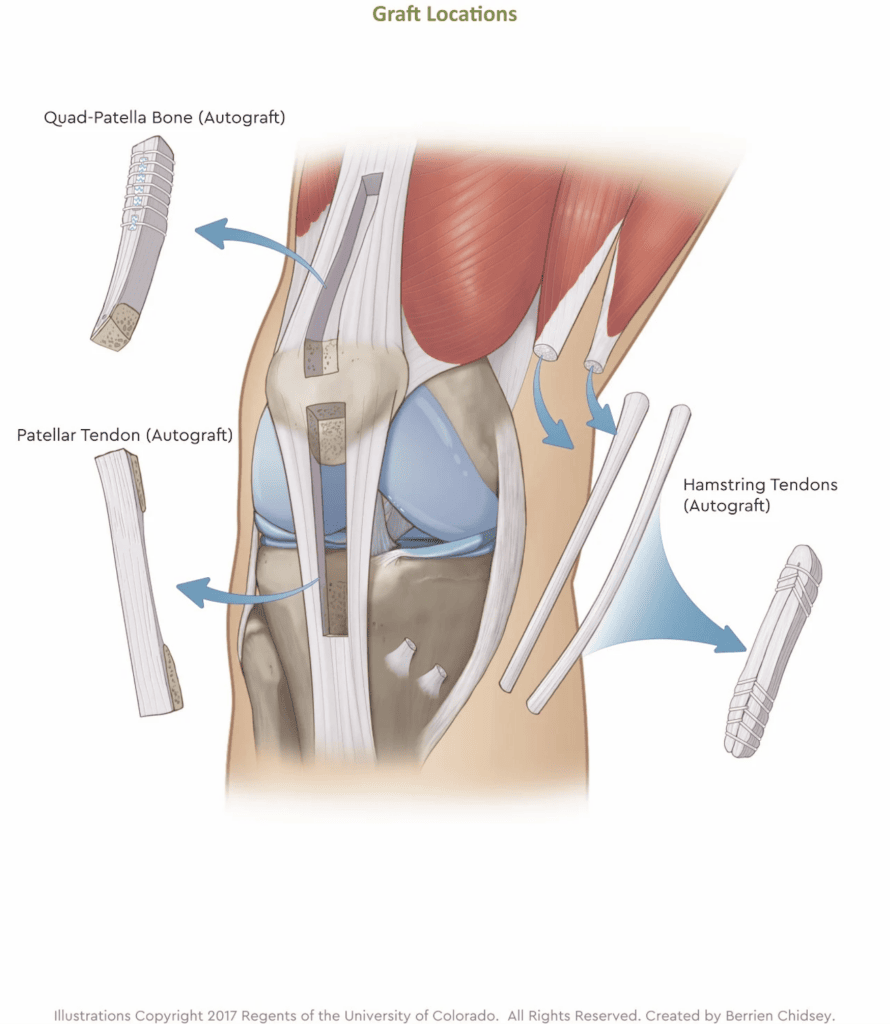
Reconstruction with Grafts: This is the most common and traditionally favored approach. It involves replacing the torn ACL with a graft. The choice of graft (autograft, allograft, or synthetic) is based on patient-specific factors.
ACL Repair: This is a less invasive method that has gained interest due to recent advancements. Repair involves reattaching the torn ligament, preserving the original ligament’s anatomy. This technique is particularly suitable for proximal tears where the tissue quality remains good. The advantage of repair is the preservation of the native ACL, which may lead to better proprioception and faster recovery. However, its applicability is limited to specific types of tears.
4.3 Graft Selection in ACL Reconstruction: Autografts - Allografts - Synthetic Grafts
A critical decision in ACL reconstruction surgery is the selection of the graft type. This choice significantly influences both the immediate success of the surgery and the long-term functionality of the knee. With options ranging from autografts (tissue from the patient’s body), allografts (donor tissue), to synthetic grafts (artificial materials), each type comes with its own set of advantages, drawbacks, and indications. Understanding the characteristics of these graft options is essential for patients and surgeons to make informed decisions that best suit the patient’s individual needs and lifestyle. Furthermore, here is an interesting study about allografts and autografts: Anterior Cruciate Ligament Grafts Choices – Alec A. Macaulay et al. – 2012.
Moreover, the 2023 study from Gerwin Haybäck et al. indicates that yearly failures rates of different surgeries are as follows: Literature search was conducted in PubMed according to Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) criteria. A total of 194 studies, which reported graft failure rates of at least one of the anterior cruciate ligament reconstruction methods mentioned above, were included in this systematic review. Overall, a total of 152,548 patients treated with an anterior cruciate ligament reconstruction were included in the calculations. Hamstring tendon autografts had a yearly graft failure rate of 1.70%, whereas the bone-patellar tendon-bone autograft group had 1.16%, the quadriceps tendon autograft group 0.72%, and the allografts 1.76%.
The findings of this meta-data study indicate that reconstructing the anterior cruciate ligament using quadriceps tendon autografts, hamstring tendon autografts, patellar tendon autografts or allografts does not show significant differences in terms of graft failure rates.
4.3.1 Autografts
These grafts, sourced from the patient’s own body, commonly involve the patellar tendon (often with a bone plug from the kneecap and shinbone), the hamstring tendon, the quadriceps tendon, or the Achilles tendon.
- Pros:
- Superior Graft Integration: Being autologous, they integrate more naturally into the body, promoting efficient healing.
- Lower Rejection Risk: The use of the patient’s own tissue reduces the likelihood of immune reactions.
- Cons:
- Donor Site Morbidity: The extraction of tissue can result in pain, weakness, or sensory changes at the harvest site.
- Longer Recovery Period: Healing is required at both the donor and graft sites, potentially prolonging rehabilitation.
- Indications: Autografts are often preferred for young, active individuals, especially athletes, due to the graft’s robustness and ability to withstand high-level physical activities.
It should however be noted that the Achilles tendon is less commonly used compared to other autograft sources. The primary reasons for its less frequent use are related to its anatomical and biomechanical properties, as well as surgeon preference and experience.
4.3.2 Allografts
Sourced from cadavers, allografts present a practical alternative to autografts in certain clinical situations.
- Pros:
- No Donor Site Morbidity: These grafts eliminate complications associated with tissue harvesting.
- Reduced Surgical Time: The absence of donor site harvesting streamlines the surgical process.
- Cons:
- Risk of Disease Transmission: Although rare, there is a potential for transmitting infections.
- Slower Integration: Allografts may incorporate more slowly into the host body, possibly delaying recovery.
- Immune Response: There’s a slight risk of immunogenic reactions to the foreign tissue.
- Indications: Suitable for older patients, those undergoing revision ACL surgeries, or patients who prefer to avoid donor site complications.
4.3.3 Synthetic Grafts
Constructed from artificial materials, synthetic grafts are considered in cases where traditional graft options are unsuitable.
- Pros:
- Immediate Strength: These grafts provide strength from the time of surgery.
- No Donor Site Concerns: Eliminates the need for tissue harvesting, averting related complications.
- Consistent Quality: Synthetic grafts offer uniform strength and size, ensuring predictability in surgical outcomes.
- Cons:
- Durability Questions: Long-term performance within the body remains a concern.
- Integration Issues: The body’s response to artificial materials can affect the graft’s integration and functionality.
- Synovial Reactions: Potential for inflammatory responses within the joint.
- Indications: Considered for patients with multiple comorbidities, limited options due to previous surgeries, or those seeking an alternative to biological grafts.
In summary, the choice of graft in ACL reconstruction is a nuanced decision, requiring a thorough understanding of the advantages and limitations of each type, and should be tailored to the individual patient’s clinical profile and specific needs. This crucial step in ACL surgery reflects the ongoing quest for optimal treatment approaches that balance biological integration, mechanical robustness, and patient-specific factors.
4.4 Arthroscopic ACL Reconstruction Surgeries: Technical Breakdown of Current Procedures
This state-of-the-art technique has become the standard for ACL surgery. It involves the insertion of an arthroscope, a small camera, through tiny incisions around the knee. This provides the surgeon with a clear view of the knee’s interior on a monitor, allowing for precise surgical maneuvers. Specialized instruments are then used to remove the damaged ACL and prepare the knee for the graft. The selected graft is then inserted and secured in place, replicating the ACL’s original anatomy as closely as possible. The advantages of arthroscopic reconstruction include less invasive surgery, reduced risk of complications, minimized scarring, and a significantly shorter recovery period compared to traditional open surgery. The technique’s precision allows for optimal graft placement and tensioning, critical for restoring knee stability and function. Postoperative rehabilitation is also enhanced, with patients often able to commence mobility exercises sooner and return to normal activities more quickly.
Let’s now explore the various graft options available in ACL reconstruction, each with its distinct characteristics and considerations. This deep dive into the pros, cons, and indications of different grafting techniques such as Patellar Tendon, Hamstring Tendon, Quadriceps Tendon Grafts, as well as Allografts and Synthetic Grafts, will provide a comprehensive understanding of their roles in optimizing surgical outcomes and patient recovery. Furthermore, here is an interesting study about the diiferent techniques: Anterior Cruciate Ligament Grafts Choices – Alec A. Macaulay et al. – 2012.
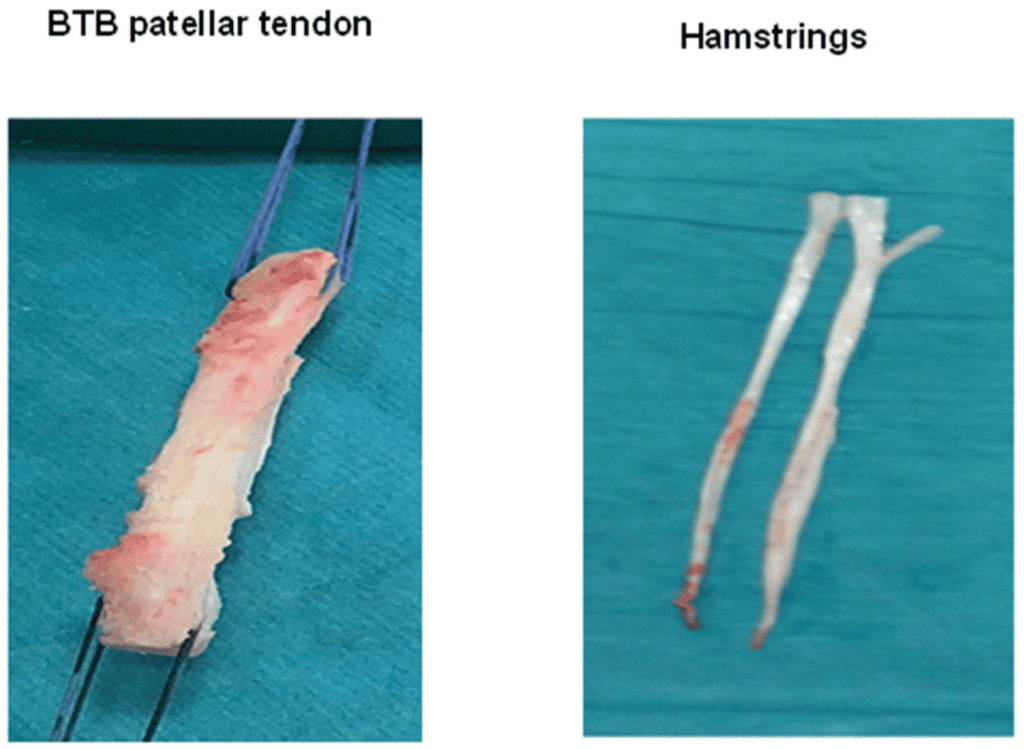
4.4.1 Bone-Patellar Tendon-Bone (BPTB) Technique
Patellar Tendon Grafts involve the utilization of the central portion of the patellar tendon, accompanied by bone plugs from both the shin (tibia) and the kneecap (patella). This technique is particularly favored in athletic populations owing to the graft’s inherent strength and resilience, mirroring the native ACL’s biomechanical properties. However, it’s important to note that this method can result in increased pain and a prolonged recovery period in the anterior knee, due to the bone plug harvesting. The robust nature of this graft makes it suitable for individuals requiring high-level knee stability, such as those involved in pivoting sports.
- High Strength and Stability: Particularly effective for athletes, offering excellent knee stability.
- Bone-to-Bone Healing: Facilitates faster and more robust graft incorporation, leading to stronger reconstruction.
- Better Proprioception: Due to the bone plug, there’s potentially improved joint awareness post-surgery.
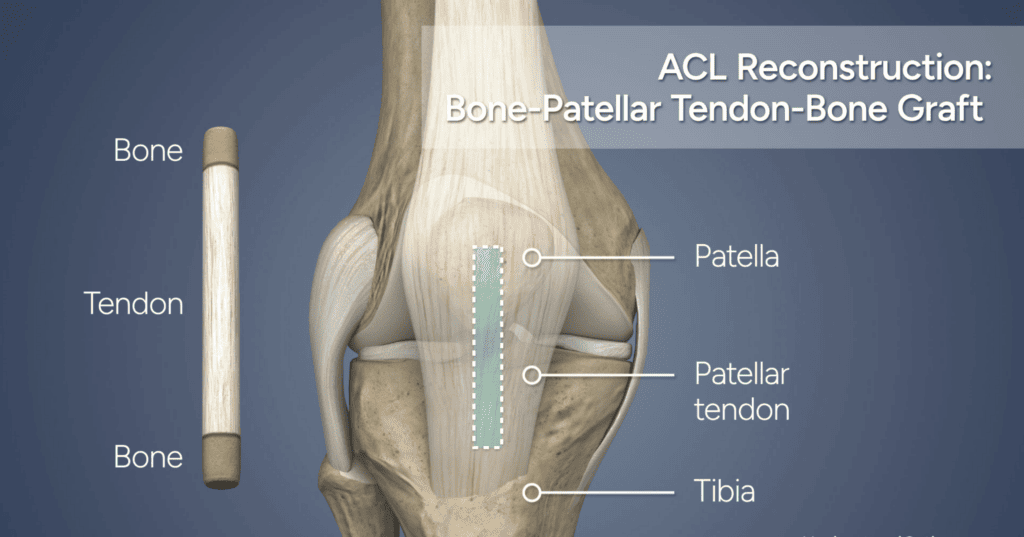
- Anterior Knee Pain and Stiffness: Increased risk of pain and stiffness in the front of the knee.
- Risk of Patellar Fracture: Due to bone plug harvesting, there’s a small risk of fracturing the kneecap.
- Postoperative Mobility Issues: Might affect the knee’s range of motion in the short term.
- Highly recommended for young, active individuals, especially athletes involved in high-impact sports, needing optimal knee stability.
4.4.2 Hamstring Tendon (HT) Graft Technique
The Hamstring Tendon Graft technique, involving the use of tendons from the hamstring muscles, is a popular choice for ACL reconstruction. This method is favored for its reduced pain at the graft site and less invasive nature. Notably, the hamstring graft is renowned for its flexibility, making it a preferred option for patients seeking a less painful recovery process. However, it’s crucial to consider that in some cases, the hamstring graft might not provide the same level of strength as the patellar tendon graft, a factor that becomes particularly important for athletes in high-impact sports.
During surgery, the hamstring graft can be prepared as either a double-strand (2-strand) or quadruple-strand (4-strand) graft. The choice between these two configurations depends on several factors, including the patient’s anatomy and the surgeon’s preference.
The 4-strand hamstring graft is commonly used as it typically provides greater strength and thickness, which is closer to the native ACL’s size. It is a technique where both the semitendinosus and gracilis tendons are used. Each tendon is folded over to create a four-strand graft, hence the term “DT4” (Double Tendon, 4 strands).This is particularly advantageous in providing the needed stability for athletes or individuals with physically demanding lifestyles.
On the other hand, the 2-strand hamstring graft may be considered in scenarios where a thinner graft is required, or in specific clinical situations based on the individual’s unique knee structure and surgical requirements. In this case, only the semitendinosus tendon is used and folded over to create a double-strand graft. This is less common and may be referred to as “DT2” (Double Tendon, 2 strands).
While the hamstring tendon graft is an excellent option for ACL reconstruction, particularly for those prioritizing comfort and a minimally invasive approach, the decision between a 2-strand or 4-strand graft configuration should be tailored to the individual’s specific needs, activity level, and surgical objectives.
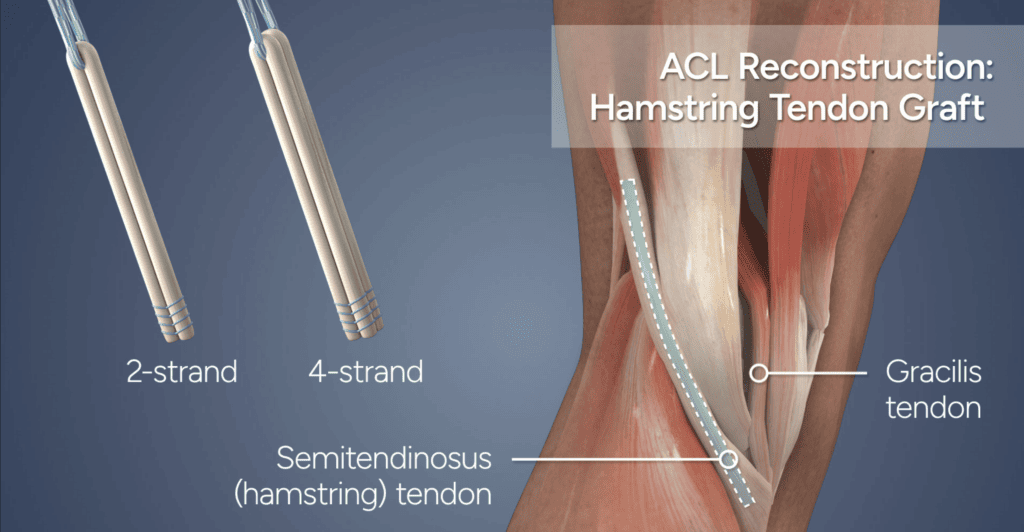
- Reduced Donor Site Pain: Lower incidence of pain at the graft site compared to patellar tendon grafts.
- Less Invasive: Involves smaller incisions and less disruption of knee structures.
- Good Functional Outcomes: Often results in good knee stability and patient satisfaction.
- Potential Graft Strength Concerns: May not provide the same level of strength and stiffness as patellar tendon grafts.
- Risk of Hamstring Weakness: Can lead to a weakening of the hamstring muscles.
- Possibility of Graft Elongation: Risk of the graft stretching over time, potentially affecting stability.
- Suitable for patients where donor site pain is a significant concern and for those not engaged in high-level pivoting sports.
4.4.3 Quadriceps Tendon Bone (QTB) Graft Technique
The Quadriceps Tendon Graft represents a modern approach in ACL reconstruction, utilizing a portion of the quadriceps tendon, which can include a bone plug. This technique is increasingly becoming a viable choice for patients who have undergone previous patellar tendon grafts or are dealing with conditions like patellar tendonitis. Its larger graft size is advantageous for better stability and is often associated with less postoperative pain than the patellar tendon graft. Gaining popularity for its versatility and efficacy, the quadriceps tendon graft is particularly suitable for patients with specific knee conditions or a history of knee surgeries.
- Versatile Graft Size: Provides a larger graft, useful in primary and revision surgeries.
- Reduced Anterior Knee Pain: Generally less painful and less stiffness compared to patellar tendon grafts.
- Good Biomechanical Properties: Offers strength and stability comparable to other autografts.
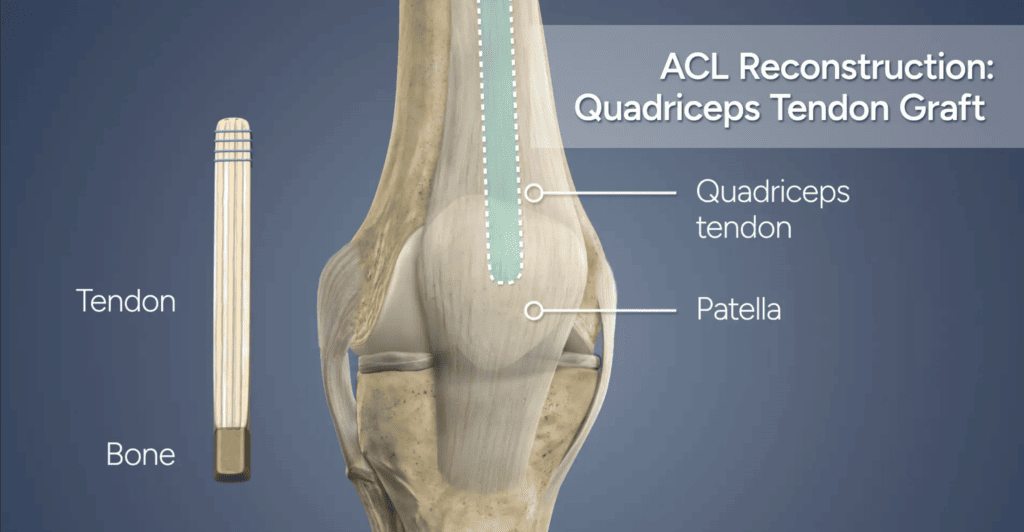
- Thigh Weakness: Can affect the performance of the quadriceps muscle.
- Limited Long-term Data: Being a newer method, it has less historical data to fully assess long-term outcomes.
- Surgical Complexity: May require more surgical skill and experience due to its relative novelty.
- Ideal for patients with previous patellar tendon grafts, patellar tendonitis, or those needing larger grafts for revision surgery.
4.4.4 Allograft Tendon Technique
Allografts offer a less invasive option in ACL reconstruction, utilizing donor tissue. The external sourcing of the graft means that there’s no need for graft harvesting from the patient’s own body, which can lead to a quicker recovery process. Allografts are commonly selected for older or less active patients, as the demands placed on the knee are typically lower in these groups. However, it is crucial to be aware of the small but present risks associated with allografts, such as disease transmission and graft rejection. These risks, though minimal, are important considerations in modern surgical planning and tissue processing.
- Reduced Recovery Time: Less invasive, allowing for faster recovery and return to activities.
- No Donor Site Complications: Eliminates pain and morbidity associated with autograft harvesting.
- Variety of Graft Choices: Offers different options in terms of size and type of tissue.
- Risk of Infection and Disease Transmission: Though minimal, the risk exists.
- Slower Integration and Healing: Can take longer to fully incorporate into the patient’s knee.
- Potential for Immune Response: Body might react to the foreign tissue, affecting graft survival.
- Commonly used in older or less active patients, or in those seeking quicker recovery times with minimal surgical impact.
4.4.5 Synthetic Graft Technique
Synthetic Grafts, made from artificial materials, are generally a choice of last resort, used when traditional graft options are not suitable or have been previously used. These grafts provide immediate strength and avoid the need for harvesting donor tissue, but there are ongoing concerns about their long-term outcomes and comparatively higher failure rates. Synthetic grafts are usually considered in complex cases where patient-specific factors or prior surgeries limit the use of more traditional autografts or allografts.
- Immediate Postoperative Stability: Provides immediate knee stability following surgery.
- No Harvesting Required: Avoids the pain and complications of donor site harvesting.
- Consistent Quality and Availability: Offers uniform strength and is readily available.
- Concerns About Long-term Outcomes: Higher failure rates and concerns about durability in the long term.
- Risk of Joint Irritation and Inflammation: Potential for adverse reactions within the knee.
- Limited Integration with Host Tissue: Can lead to issues with graft incorporation and knee biomechanics.
- Generally considered in complex clinical scenarios or for patients who have exhausted other graft options due to previous surgeries or comorbidities.
4.5 Single Bundle vs. Double Bundle Reconstruction
In ACL reconstruction, whether using HT, BPTB, QTB or Synthetic graft techniques, surgeons can opt for either Single Bundle or Double Bundle Reconstruction, each with distinct advantages.
Single Bundle Reconstruction focuses on replacing the torn ACL with a single graft. This technique is more traditional and widely used due to its simplicity and effectiveness in restoring anterior-posterior stability. However, it may not fully replicate the ACL’s complex anatomy, particularly its rotational stability.
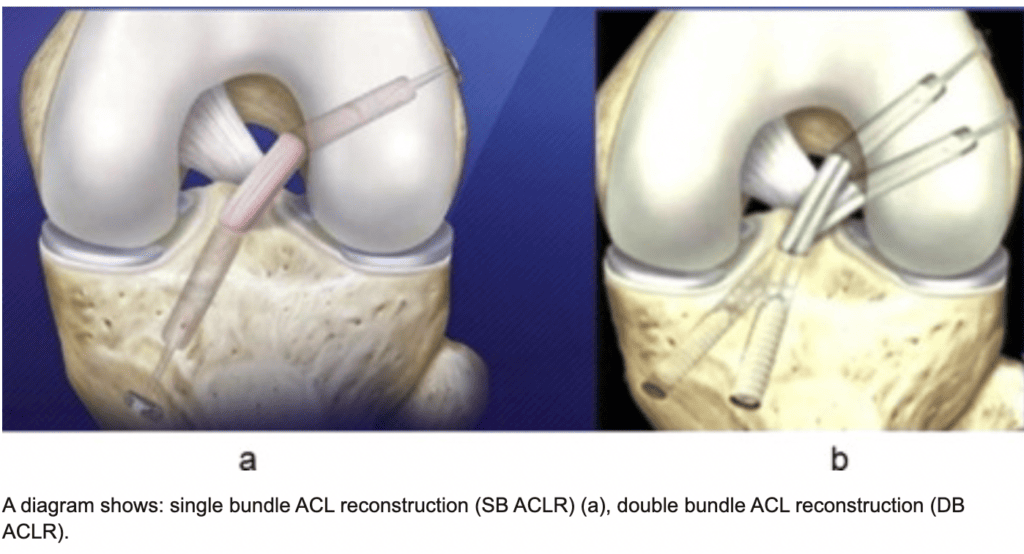
Double Bundle Reconstruction, on the other hand, aims to more closely mimic the ACL’s natural anatomy by using two separate grafts to reconstruct both the anteromedial (AM) and posterolateral (PL) bundles of the ACL. This approach is thought to provide better rotational stability and may be particularly beneficial for patients with high functional demands or those involved in pivoting sports. However, it is technically more complex and may have a longer recovery time.
The choice between these techniques depends on various factors, including the patient’s anatomy, activity level, and the surgeon’s expertise. Recent studies suggest that while double bundle reconstruction may offer some biomechanical advantages (Read Lin Study 2022), both techniques generally yield similar outcomes in terms of knee stability and patient satisfaction.
In conclusion, both single and double bundle ACL reconstructions have their merits, and the decision should be tailored to each patient’s specific needs and circumstances.
4.6 Tunnel Surgery Techniques
In ACL reconstruction, selecting the right tunnel technique is vital for successful outcomes. This choice significantly influences the knee’s stability and function post-surgery. Techniques vary to best replicate the ACL’s natural positioning, tailored to individual anatomy and surgical goals. Factors influencing the choice include specific knee characteristics and recovery expectations, aiming for optimal stability and mobility. The main different methods used nowadays are:
- Anteromedial Portal Technique
- Outside-In Technique
- All-Inside Technique
- Over-the-Top Technique
- TransPortal Technique
- Transtibial Technique
The transtibial technique involves drilling through the tibia to create a pathway for the graft. The anteromedial portal technique offers a more anatomical approach, allowing for better alignment with the ACL’s natural orientation. The outside-in technique provides precise control over the tunnel’s exit and entry points. The all-inside technique is less invasive, reducing the amount of bone removed and potentially speeding up recovery. The over-the-top method circumvents traditional drilling, offering an alternative for graft placement. Lastly, the transPortal technique optimizes graft positioning through precise tunnel creation, preserving knee anatomy and function. Each technique has its specific advantages, tailored to the patient’s anatomy and the surgeon’s expertise, with the goal of restoring knee stability and functionality while minimizing recovery time.
Should you be interested in additional info about the different tunnel surgery techniques, we invite you to take a look at our article dedicated to the topic: Click here to read it.
4.7 Technical Aspects of ACL Surgery
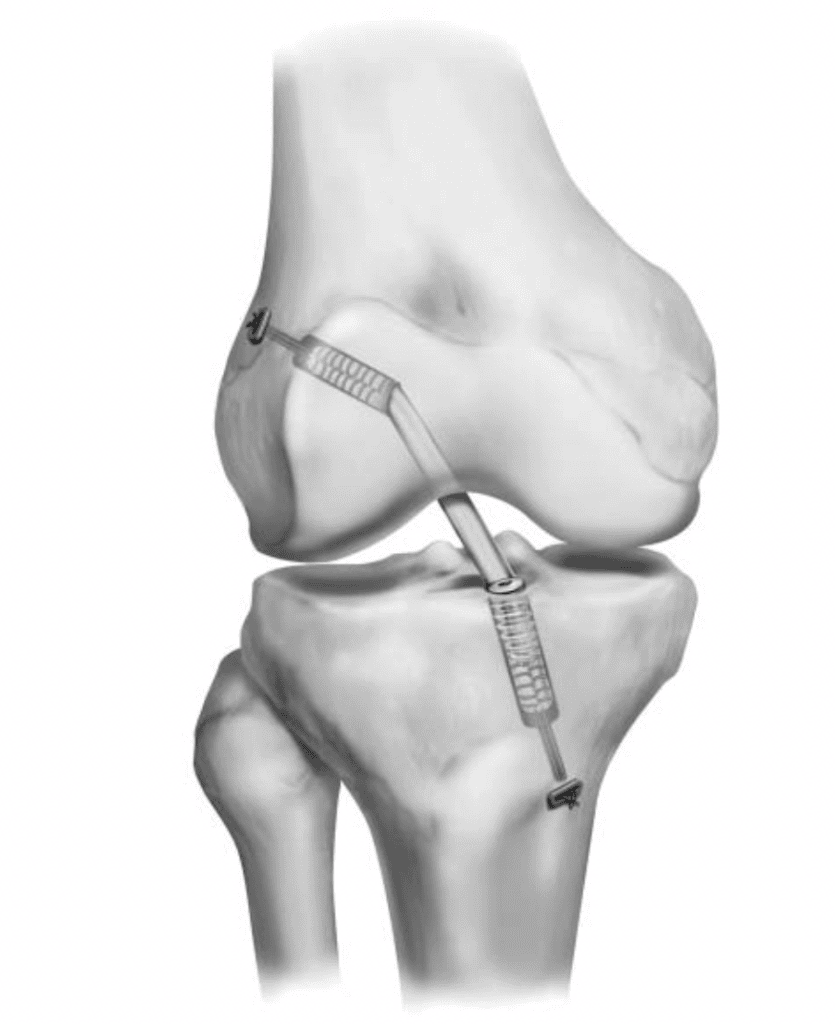
Successful ACL surgery is contingent upon several key technical aspects. These include precise anatomical graft placement, accurate tunnel positioning, optimal graft tensioning, and secure graft fixation. Each of these elements plays a crucial role in ensuring the reconstructed ligament’s stability and functionality. Meticulous attention to detail in these areas is essential for the overall success of the procedure and the long-term health and mobility of the knee joint.
Anatomical Graft Placement: This involves positioning the graft so that it mimics the natural anatomy of the original ACL. Correct placement is crucial for restoring the natural kinematics of the knee joint. Surgeons must carefully measure and place the graft at the anatomical insertion points of the ACL to ensure proper joint mechanics.
Proper Tunnel Positioning: Creating tunnels in the tibia and femur for graft placement is a delicate process. The tunnels must be accurately aligned to avoid impingement or graft stretching, which can compromise the stability and longevity of the reconstruction.
Optimal Graft Tensioning: The graft must be tensioned correctly to provide sufficient stability without overly constraining the knee’s normal range of motion. This balance is critical to prevent either laxity or excessive tightness, both of which can adversely affect knee function.
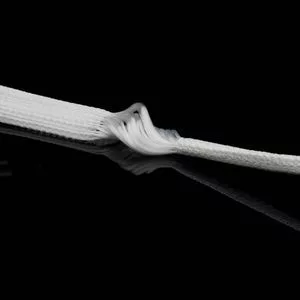
Secure Graft Fixation: Ensuring that the graft is securely fixed in place is vital for its integration into the bone. Various fixation devices and techniques are employed, including screws and endobuttons, which must be chosen and applied based on the graft type and individual patient factors.
4.8 Innovations and Advancements
The field of ACL reconstruction is dynamic and constantly evolving, with ongoing innovations significantly enhancing surgical outcomes. These advancements encompass new surgical techniques, improved equipment, and evolving fixation methods, all contributing to more precise and effective procedures. This continuous development not only refines the current practices but also opens up new possibilities for treating ACL injuries, ultimately leading to better patient recovery experiences and long-term results.
Technological Advancements: Developments in surgical instruments and imaging technologies have greatly improved the precision of ACL surgeries. Computer-assisted surgery and the use of robotics are examples of such advancements.
New Fixation Devices: There is continuous evolution in the types of fixation devices used, with newer models designed to provide stronger and more reliable graft fixation while minimizing tissue damage.
Biological Enhancements: Research into biological methods to improve graft healing and integration is ongoing. This includes techniques like growth factor application and stem cell therapies, which could significantly improve recovery times and outcomes.
5. The Surgical Procedure
The arthroscopic procedure for ACL reconstruction is a meticulously planned operation that involves several critical steps, both before and after the surgery, to ensure optimal outcomes.
5.1 Pre-operative Preparations
Before the surgery, patients undergo a comprehensive evaluation to ensure they are suitable candidates for the procedure. This includes a detailed review of their medical history, physical examinations, and imaging tests such as MRI. In addition to MRI, a dynamic assessment using an arthrometer is often performed. The arthrometer test is crucial as it mimics real-life stresses on the knee, offering valuable insights into the knee’s functional stability that static images like MRI cannot provide. Patients receive guidance on what to expect before and after the surgery, including fasting instructions and adjustments to their current medication regimen. Prior to the operation, the surgical area is carefully marked and thoroughly cleaned to minimize the risk of infection.
5.2 Step-by-Step Walkthrough
- Anesthesia: The patient is administered either general anesthesia or a regional nerve block.
- Incision and Arthroscope Insertion: Small incisions are made around the knee, through which the arthroscope, a tiny camera, is inserted.
- Assessment of Damage: The surgeon examines the ACL and other knee structures for any additional damage.
- Graft Preparation: Concurrently, the chosen graft (autograft, allograft, or synthetic) is prepared for insertion.
- Tunnel Creation: Precision-drilled tunnels in the tibia and femur are made to accommodate the new graft.
- Graft Insertion: The graft is then inserted through these tunnels, positioning it anatomically to replicate the original ACL.
- Graft Fixation: The graft is secured in place using screws or other fixation devices.
- Final Inspection and Closure: The knee is inspected for proper graft placement, range of motion, and the incisions are then closed.

5.3 Post-operative Expectations
Post-surgery, patients can expect some pain and swelling, which is managed through medications and ice therapy. Rehabilitation starts almost immediately with mobility exercises to prevent stiffness. Physical therapy is crucial for gradual strengthening and return to normal activities. The recovery timeline varies, but most patients can resume light activities within a few weeks and full sports activities in 6-12 months, depending on individual progress.
5.4 Role of Technology in Enhancing Outcomes
Advanced technology plays a pivotal role in enhancing surgical precision and outcomes. Computer-assisted surgery, dynamic Assessments with Arthrometers, 3D imaging, and improved arthroscopic equipment allow for more accurate graft placement and tunnel positioning. These technologies contribute to reduced complications, faster recovery, and more consistent results across different patient cases.
6. Recovery and Rehabilitation

The journey to recovery and rehabilitation following ACL surgery is a structured and essential process, varying significantly based on the type of surgery performed and the individual patient’s characteristics.
This path is divided into distinct phases, each with specific goals and activities designed to ensure a safe and effective return to full function. The rehabilitation process is tailored to the individual’s needs, taking into account the specific surgical technique used and the patient’s overall health and activity level. Understanding these phases, along with the importance of physical therapy and long-term care strategies, is crucial in preventing re-injury and ensuring a successful return to daily activities and sports. Let’s explore the detailed phases of recovery and the critical role of rehabilitation in the ACL surgery journey.
6.1 Phases of Recovery Post-ACL Surgery
If you want to read more details about the Recovery phase, you can read another article on our website: Torn ACL Recovery Time: Proven Techniques for Faster and Safer Recovery.
Navigating through the recovery and rehabilitation process post-ACL surgery is a critical journey toward regaining knee strength, stability, and functionality. The complete recovery process lasts 2 years but it should be noted that the first 6 month is the crucial phase in the recovery phase of an ACL Reconstruction surgery.
From the initial stages of managing pain and swelling to the advanced phase of returning to sports and regular activities, understanding these steps is essential for a successful recovery. The process is comprehensive, involving both physical therapy and gradual reconditioning of the knee, ensuring patients can achieve their pre-injury level of activity and quality of life.
- Immediate Postoperative Phase (0-2 Weeks): Focuses on reducing swelling, managing pain, and protecting the graft. Involves the use of crutches and possibly a knee brace.
- Early Rehabilitation Phase (2-6 Weeks): Emphasizes regaining range of motion and gentle strengthening, with gradual introduction of weight-bearing activities.
- Intermediate Rehabilitation Phase (6-12 Weeks): Involves more advanced strengthening exercises, balance, and proprioception training.
- Advanced Rehabilitation Phase (3-6 Months): Includes rigorous activities and sport-specific exercises to restore strength, endurance, and flexibility.
- Return to Activity Phase (6 Months and Beyond): Focuses on a gradual return to normal activities and sports, ensuring adequate knee strength and stability.
The journey through recovery and rehabilitation post-ACL surgery is a crucial phase, underscored by several studies focusing on dynamic assessments of the knee. Research by Forelli (2023), Semay et al. (2016), Nouveau-Robert and Viel (2017), and Pouderoux et al. (2019) all emphasize the value of using dynamic arthrometers like the Dyneelax/GNRB for postoperative follow-ups. These tools provide valuable insights into the ligament’s healing process and knee stability, offering a comprehensive view of recovery beyond traditional methods.
6.2 Importance and Goals of Physical Therapy
Physical therapy (PT) is a cornerstone of successful recovery from ACL surgery. It plays a pivotal role in restoring knee function, strength, and flexibility. The primary goals of PT post-surgery include:
- Reducing Post-Surgery Complications: Effective PT helps in mitigating risks such as stiffness, excessive scar tissue formation, and loss of range of motion.
- Minimizing Pain: Through targeted exercises and modalities, PT aids in managing and gradually reducing postoperative pain.
- Restoring Normal Movement Patterns: Therapists work on retraining the knee to move in a way that mimics pre-injury movement, which is essential for returning to normal activities.
- Preventing Muscle Atrophy: PT includes strength training exercises that focus on not just the knee, but also the surrounding muscle groups to prevent atrophy and promote balanced muscle development.
- Ensuring a Safe and Efficient Return to Activities: A gradual and structured increase in activity levels ensures patients return to their daily activities and sports safely, minimizing the risk of re-injury.
A tailored physical therapy program is crucial, considering the individual’s specific surgery, lifestyle, and activity goals. It’s a progressive process, starting with basic exercises and gradually moving to more complex and demanding activities.
6.3 Long-term Care and Prevention of Re-Injury
Long-term care post-ACL reconstruction is vital for maintaining the health and functionality of the knee. Key components include:
- Ongoing Exercises: Regular exercises to maintain knee strength and flexibility are essential. These may include strength training, flexibility exercises, and activities that enhance joint mobility.
- Healthy Lifestyle: A balanced diet, weight management, and overall healthy lifestyle choices play a significant role in supporting joint health and recovery.
- Injury Prevention Strategies:
- Regular Arthrometer Testing: Periodic assessments using an arthrometer can provide valuable insights into knee stability and function, helping to monitor progress and prevent potential issues. It helps getting feedback about the ACL graft during the months following surgery. This enables to provide personnalised rehab programs for each patient.
- Neuromuscular Training: Improves coordination and balance, reducing the risk of awkward movements that can lead to re-injury.
- Proper Technique in Sports: Learning and maintaining the correct techniques in sports activities is crucial to avoid putting undue stress on the knee.
- Regular Physical Activity: Consistent physical activity helps in maintaining joint health and overall physical fitness.

Long-term care post-ACL reconstruction is vital for maintaining the health and functionality of the knee. Key components include:
- Ongoing Exercises: Regular exercises to maintain knee strength and flexibility are essential. These may include strength training, flexibility exercises, and activities that enhance joint mobility.
- Healthy Lifestyle: A balanced diet, weight management, and overall healthy lifestyle choices play a significant role in supporting joint health and recovery.
- Regular Follow-Up: Ongoing check-ups with healthcare providers are important to monitor recovery progress and address any emerging concerns.
- Focus on Knee Health: Emphasis should always be on practices that promote knee health and prevent future injuries, including wearing appropriate sports gear and avoiding high-risk activities without proper preparation.
Long-term care and prevention strategies are key in ensuring not just a full recovery but also in maintaining an active and healthy lifestyle post-recovery.
7. Risks and Complications
ACL surgery, like any surgical procedure, carries potential risks and complications. These can be categorized into common and rare occurrences.
7.1 Common Complications

- Infection: Though rare, infections can occur at the incision site or within the knee joint.
- Blood Clots: Patients may be at risk of developing blood clots in the leg veins, known as deep vein thrombosis (DVT).
- Graft Failure: The graft may fail to integrate properly or could rupture, necessitating additional surgery.
- Knee Stiffness and Pain: Some patients may experience stiffness and pain in the knee, particularly around the graft harvest site.
7.2 Rare Complications
- Nerve Damage: There’s a small risk of damage to the nerves around the knee, which can lead to numbness or altered sensation.
- Arthrofibrosis: A condition where excessive scar tissue forms in the knee, leading to restricted movement.
7.3 Strategies for Risk Minimization and Management
- Preoperative Planning: Thorough assessment and planning by the surgical team to identify potential risks.
- Postoperative Care: Strict adherence to postoperative care instructions, including wound care and medication management, to prevent infection and blood clots.
- Physical Therapy: Engaging in physical therapy early and consistently to prevent stiffness and improve knee function.
- Regular Follow-up: Keeping regular follow-up appointments with the surgeon to monitor the knee’s healing and address any concerns promptly.
- Patient Education: Educating patients on signs of complications, such as increased pain, swelling, or changes in wound appearance, is crucial for early detection and treatment.
Effective management and minimization of risks involve a combination of careful surgical technique, diligent postoperative care, and active patient participation in the recovery process.
8. Success Rates and Outcomes - Can an ACL Reconstruction Fail?
ACL reconstruction surgery, while generally successful, has outcomes that are influenced by a range of factors. These include the surgical technique used, the type of graft selected, the rehabilitation performed and individual patient characteristics. Understanding the variability in success rates, as well as the potential for complications, is crucial for patients considering this procedure.
8.1 Success Rates
The success rate of ACL surgery varies based on several factors. Focusing on the ACL graft, there is a potential for retearing, which might necessitate further surgery. Factors influencing the rate of retearing include the nature of the study, its duration, and measurement metrics. The likelihood of retears rises over time. Some notable statistics are:
- The probability of a second ACL injury within 24 months after ACL reconstruction and resuming sports activities is sixfold higher than in individuals without prior ACL issues (Mark V. Paterno et al. – 2013).
- At a five-year mark post-surgery, 12% of patients have experienced another ACL injury(Salmon L et al. – 2005) .
- After 15 years following the initial ACL surgery, the rate of a second injury ranges between 29% and 34% (Leys T et al. – 2012).
- Individuals younger than 25 are four times more prone to retearing their ACL after surgery compared to those older than 25 (Kamien PM et al. – 2013).
8.2 Complications and Challenges
The success rate of ACL surgery is not only about the retear rate but also includes considerations like knee stability, performance, and risk of arthritis. Surgically reconstructed ACLs often have a steeper angle due to technical constraints, potentially leading to increased arthritis. Moreover, replacing the native ACL’s two bundles with a single bundle graft can cause knee instability.
Post-surgery, muscle control, performance, and balance may be compromised, with many athletes struggling to return to their pre-surgery performance levels. A study showed a threefold increase in osteoarthritis in operated knees compared to healthy knees after 14 years (Barenius B et al. – 2014).
8.3 Can a teenager have ACL surgery?
Teenagers and growing children can undergo ACL surgery, though the approach differs from that used for adults. Young athletes, particularly those who are still growing, require specialized surgical methods.
Older teenagers, closer to adult size, can successfully undergo the standard ACL reconstruction procedure. However, performing this surgery on younger children, whose growth plates are still open, presents challenges. The traditional adult method can potentially harm these growth plates, leading to uneven limb growth or deformities. In the past, surgeons often delayed ACL surgery in children until their growth was complete, or they used less anatomically precise techniques.
Recent advancements in surgical techniques now offer several options for treating ACL injuries in young children and adolescents. A notable method, developed at HSS, is the All-Inside, All-Epiphyseal Reconstruction (AE). This approach is akin to the adult ACL surgery but incorporates new technologies and intraoperative X-rays. These innovations allow surgeons to position the ACL graft in the knee accurately, avoiding interference with the adjacent growth plates. Performed arthroscopically, this technique results in a reconstruction that closely mimics the natural ACL and has a high success rate in returning young athletes to sports. This is particularly beneficial for child athletes who would otherwise have to cease playing sports until they reached full growth.
9. Lifestyle Adjustments Post-Surgery
Post ACL surgery, long-term lifestyle and activity adjustments are often necessary to ensure optimal knee health and prevent further injuries. These adjustments play a crucial role in maintaining the benefits of the surgery over time.

Activity Modification: Patients may need to modify their activities to reduce stress on the knee. This could involve choosing low-impact exercises like swimming or cycling over high-impact sports.
Regular Exercise and Strength Training: Consistent exercise to maintain overall fitness and specific strength training for the muscles around the knee help in supporting the joint and preventing re-injury.
Weight Management: Maintaining a healthy weight is essential to reduce the strain on the knee. Overweight individuals are encouraged to adopt a healthy diet and exercise routine.
Ergonomic Adjustments: For those with physically demanding jobs, ergonomic adjustments may be necessary to reduce the risk of knee strain.
Adaptive Strategies for Athletes: Athletes, especially those in high-impact sports, might need to adjust their training routines. Incorporating more knee-strengthening exercises, using protective gear, and potentially altering their sports techniques can be beneficial.
Use of Supportive Devices: In some cases, using knee braces or orthotics as a preventive measure during high-risk activities can be helpful.
Regular Medical Check-ups: Ongoing consultations with healthcare providers are important for monitoring knee health and addressing any concerns promptly.
Mental Health Considerations: Adjusting to a new lifestyle post-surgery can be challenging. Seeking support from counselors or support groups can be beneficial in managing any psychological impacts.
In summary, post-surgery lifestyle adjustments are key to maintaining knee health and preventing further injuries. These changes, coupled with a commitment to regular physical care and monitoring, enable individuals to lead active and fulfilling lives post ACL reconstruction.
Conclusion
Understanding the complexities of ACL surgery is essential for anyone facing this medical journey. From the initial decision-making about the type of surgery, to the intricate details of the surgical procedure, and the comprehensive process of recovery and rehabilitation, each aspect plays a critical role. It’s a journey that requires a clear understanding of the potential risks, the importance of rehabilitation, and the long-term lifestyle adjustments necessary for optimal knee health.
However, it’s crucial to remember that each individual’s journey is unique. Personalized medical advice from healthcare professionals is indispensable. They can provide tailored recommendations that take into account the patient’s specific circumstances, medical history, and lifestyle. This professional guidance is crucial in navigating the nuances of ACL surgery and recovery.
Ultimately, empowerment through education, combined with expert medical advice, is key to a successful outcome. Patients are encouraged to engage actively in their healthcare decisions, ask questions, and fully understand each step of the process. By doing so, they can approach their ACL surgery and recovery with confidence, supported by the knowledge and expertise of their medical team.
Medical References
- Martha M. Murray (2021). Optimizing outcomes of ACL surgery—Is autograft reconstruction the only reasonable option DOI: 10.1002/jor.25128
- Cojean, T., Batailler, C., Robert, H., Cheze, L. (2023). GNRB® laximeter with magnetic resonance imaging in clinical practice for complete and partial anterior cruciate ligament tears detection: A prospective diagnostic study with arthroscopic validation on 214 patients. The Knee, 42, 373-381. DOI: 10.1016/j.knee.2023.03.017
- Paterno, M. V., Rauh, M., Schmitt, L. C., Ford, K. R., Hewett, T. E. (2013). Incidence of Second Anterior Cruciate Ligament (ACL) Injury 2 Years after Primary ACL Reconstruction and Return to Sport. DOI:10.1177/2325967113S00002
- Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K (2005). Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthroscopy. 2005;21(8):948-57. DOI: 10.1016/j.arthro.2005.04.110.
- Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. (2012) Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595-605. DOI: 10.1177/0363546511430375.
- Kamien PM, Hydrick JM, Replogle WH, Go LT, Barrett GR. (2013) Age, graft size, and Tegner activity level as predictors of failure in anterior cruciate ligament reconstruction with hamstring autograft. Am J Sports Med. 2013;41(8):1808-12. DOI: 10.1177/0363546513493896.
- Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomised controlled trial. Am J Sports Med. 2014;42(5):1049-57. DOI: 10.1177/0363546514526139.
- Macaulay, A. A., Perfetti, D. C., Levine, W. N. (2011). Anterior Cruciate Ligament Graft Choices. DOI: 10.1177/1941738111409890.
- Semay, B., Rambaud, A., Philippot, R., & Edouard, P. (2016). Evolution of the Anteroposterior Laxity by GNRB at 6, 9, and 12 Months Post-Surgical Anterior Cruciate Ligament Reconstruction. DOI: 10.1016/j.rehab.2016.07.045.
- Nouveau, S., Robert, H., & Viel, T. (2017). ACL Grafts Compliance During Time: Influence of Early Solicitations on the Final Stiffness of the Graft after Surgery. Journal of Orthopedic Research and Physiotherapy, 3(1), 035. DOI: 10.24966/ORP-2052/100035.
- Forelli (2023). After Surgery Rehab Post-Op. International Journal of Sports Physical Therapy. Submitted: October 10, 2022. Accepted: January 15, 2023. DOI: 10.26603/001c.73031.
- Pouderoux, T., et al. (2019). Joint laxity and graft compliance increase during the first year after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. DOI: 10.1007/s00167-019-05711-z
- Lin, L., Wang, H., Wang, Y., Wang, J., Liu, Y., Yu, J. (2022). Double-Bundle Versus Single-Bundle Anterior Cruciate Ligament Reconstruction in Patients With Significant Passive Anterior Tibial Subluxation. DOI: 10.1177/03635465211072562
- Haybäck, G., Raas, C., Rosenberger, R. (2021). Failure rates of common grafts used in ACL reconstructions: a systematic review of studies published in the last decade. DOI: 10.1007/s00402-021-04147-w
- Forsythe B, Lu Y, Agarwalla A, Ezuma CO, Patel BH, Nwachukwu BU, Beletsky A, Chahla J, Kym CR, Yanke AB, Cole BJ, Bush-Joseph CA, Bach BR, Verma NN. (2021). Delaying ACL reconstruction beyond 6 months from injury impacts likelihood for clinically significant outcome improvement. Knee, 33, 290-297. DOI: 10.1016/j.knee.2021.10.010