Introduction
Anterior Cruciate Ligament (ACL) injuries are a prevalent concern in orthopedic and sports medicine, particularly among athletes. The ACL, a crucial stabilizer of the knee joint, is susceptible to tears and ruptures, often requiring comprehensive diagnostic and therapeutic approaches. Traditionally, the diagnosis of ACL injuries involves a tiered approach, starting with a clinical examination by an experienced practitioner. This initial assessment typically includes physical tests like the Lachman test, the pivot-shift test, and the anterior drawer test, which provide preliminary insights into the integrity of the ACL. Following this, Magnetic Resonance Imaging (MRI), the gold standard in imaging, helps confirm the diagnosis through its detailed visualization of soft tissue structures.
However, the reliance on static MRI images is a notable limitation. It fails to capture the dynamic stresses experienced by the knee joint in real-life activities. In the dynamic environment of sports and daily activities, the knee joint experiences various stresses and movements that static images cannot capture. This is where dynamic testing technologies, such as GNRB/Dyneelax, become crucial. These systems offer a functional evaluation of the knee, providing vital insights, especially in detecting partial ACL tears, which are often challenging to diagnose with MRI. By simulating the movements and stresses the knee typically undergoes, these tests can offer valuable insights into the joint’s functional stability.
Beyond diagnosis, dynamic testing also plays a pivotal role in the rehabilitation process after ACL reconstruction surgery (ACLR). Monitoring the functional recovery of the knee joint, dynamic testing helps in tailoring rehabilitation protocols and ensuring safe and effective recovery. This aspect is particularly important as it addresses the patient’s return to sports or daily activities, ensuring the knee can withstand the required physical demands.
Integrating dynamic testing both pre- and post-surgery represents a significant advancement in personalised ACL injury management. It offers a more comprehensive understanding of the injury and recovery process, facilitating a tailored approach to treatment and rehabilitation. This evolution in diagnostic and therapeutic strategies underscores the importance of dynamic testing in contemporary orthopedic and sports medicine practices.
In this article, we will dive into the complex world of dynamic knee testing, both in the context of initial ACL injury diagnosis and during the critical phase of post-surgery rehabilitation. To substantiate our discussions, we will provide links to scientific studies with their DOIs, offering a robust evidence base for our insights.
1. Background and Current Practices

The diagnosis of Anterior Cruciate Ligament (ACL) injuries involves a multifaceted approach, rooted in both clinical and imaging techniques. Initially, clinical examination is fundamental. This includes physical tests such as the Lachman test, which assesses anterior tibial translation and end-point quality, the pivot-shift test, indicative of rotational instability, and the anterior drawer test. These examinations, reliant on the clinician’s experience, offer initial insights into the potential of an ACL injury.
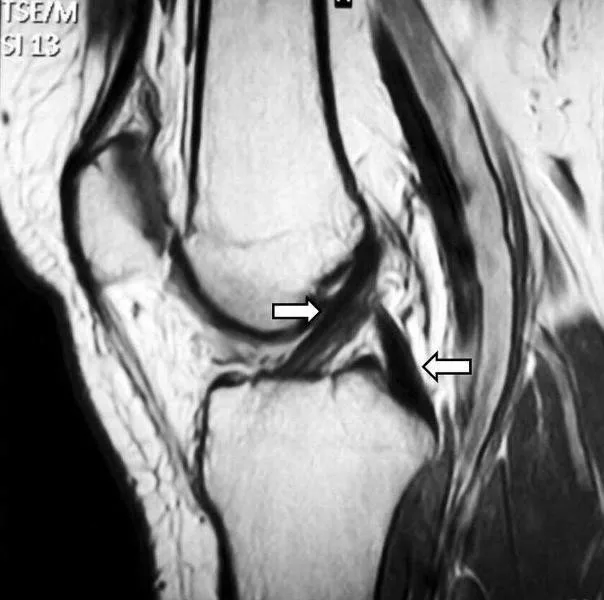
Following clinical suspicion, the diagnostic pathway typically advances to Magnetic Resonance Imaging (MRI). MRI is renowned for its high sensitivity and specificity in visualising the knee’s soft tissue structures, including the ACL. It provides detailed images that are critical for confirming the diagnosis and planning subsequent treatments, such as ACL reconstruction surgery in cases of complete ruptures.
However, this approach has significant limitations. The static nature of MRI is a major concern, as it doesn’t simulate the dynamic stresses experienced by the knee. This shortcoming is particularly pronounced in detecting partial ACL tears, where dynamic instability isn’t evident in static images. Another limitation arises in acute injury settings, where bleeding and swelling can interfere with MRI accuracy. In such cases, the presence of blood and fluid in the joint can obscure the view, leading to potential misdiagnosis or underestimation of the injury’s severity.
These constraints highlight the necessity for a more dynamic, functional diagnostic tool that can accurately replicate and assess the knee’s movements and stresses. Such a tool would enhance detection of subtle injuries like partial ACL tears and lead to more precise and effective treatment strategies.
Another area where current practices fall short is in providing feedback on the graft’s resistance during rehabilitation. The dynamic testing offered by our robotic arthrometer can fill this gap, offering crucial insights into the graft’s condition during the rehab process.
In exploring dynamic knee testing, we aim to demonstrate how it could effectively address these shortcomings of traditional diagnostic methods.
2. The Case for Dynamic Knee Testing
Dynamic knee testing, a significant advancement in orthopedic diagnostics, offers comprehensive assessments of knee joint behavior under realistic conditions. This technology is crucial in understanding and managing ACL injuries, where traditional methods have limitations. We explore three innovative aspects of dynamic knee testing, focusing on the DYNEELAX® and GNRB® arthrometers.
2.1 Automated Anterior/Posterior Tibial Translation Analysis
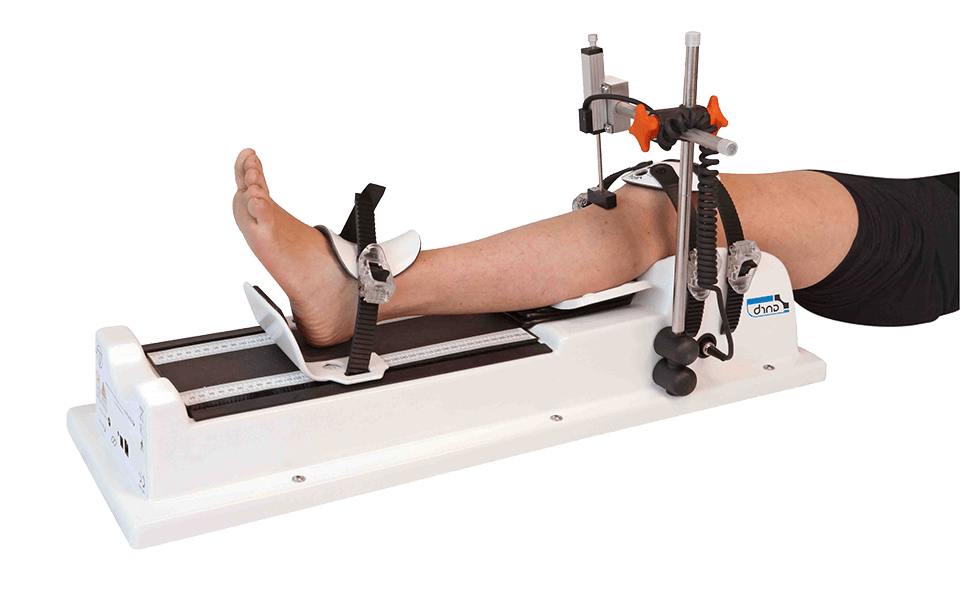
Automated Anterior/Posterior Tibial Translation Analysis, a technique akin to the manual Lachman test, represents a significant leap in ACL and PCL diagnostics. Unlike the manual test, which depends on the clinician’s skill and experience, this automated method uses devices like the GNRB® robotic arthrometer to provide highly accurate and reproducible measurements. This precision stems from the machine’s ability to consistently apply force and measure the resulting tibial translation, eliminating the subjectivity inherent in manual examinations.
Historically, manual arthrometers like the KT1000 have been used to assess knee laxity. However, these devices, while a step forward from purely manual tests, still lacked the precision and consistency of fully automated systems. The GNRB® arthrometer, through its automated process, offers a more objective assessment, crucial for detecting subtle yet clinically significant differences in knee laxity.
In terms of validating the effectiveness of the GNRB® in measuring ACL integrity, several studies stand out. For instance, the research conducted by Théo Cojean et al. in 2023 demonstrates the superiority of the GNRB® over MRI in detecting partial ACL tears. The study indicates that while MRI showed a sensitivity of 29.51% for partial tears, the GNRB® achieved a significantly higher sensitivity of 73.77% at a force of 134 N. This stark contrast highlights the GNRB’s ability to detect injuries that MRI might miss, emphasizing its role in comprehensive ACL assessment.
Further validating the GNRB’s efficacy, a study by Miha Magdič et al. in 2022 focused on the intra-rater reliability of the GNRB® arthrometer in measuring knee anterior laxity. The study’s results showed good intra-rater reliability for measurements at forces of 134 N and 200 N. This level of reliability, demonstrated in a large sample size, underscores the consistency and accuracy of the GNRB® in assessing knee laxity, a crucial factor in diagnosing ACL integrity. The emphasis on standardized measurement protocols further enhances the reliability of the results, ensuring that the GNRB® provides dependable and repeatable measurements in clinical settings.
Additional research further validates the GNRB® arthrometer’s effectiveness. The 2015 study by Klouche et al. demonstrated its diagnostic value in relation to pressure load for complete ACL tears. This prospective case-control study confirmed the GNRB®’s accuracy and reliability in differentiating complete tears from healthy ACLs. Additionally, Jenny’s 2017 research provided experimental validation of the GNRB® for measuring anterior tibial translation, supporting its use as a reliable diagnostic tool. Lastly, Kayla Smith’s 2023 study on the reliability of the GNRB® in measuring ACL stiffness and laxity further emphasized its clinical utility, underscoring its role in enhancing ACL injury diagnostics and treatment planning. These studies collectively showcase the GNRB® arthrometer as a pivotal advancement in ACL injury assessment.
2.2 Medial/Lateral Tibial Rotation Assessments
Rotational stability is a key aspect of knee joint mechanics, especially in the context of ACL injuries. While the pivot shift test is a traditional method for assessing rotational instability, its subjective nature can lead to variability in results. The introduction of the Dyneelax arthrometer, the only device capable of precisely measuring rotational stability, marks a significant advancement in dynamic knee testing.
This robotic arthrometer offers an objective, quantifiable approach to evaluating medial and lateral knee rotation. Its precise measurements provide a more accurate assessment of rotational stability, surpassing the limitations of manual testing.

By incorporating the DYNEELAX® and GNRB® in diagnostic and rehabilitation protocols, clinicians can achieve a more comprehensive understanding of knee mechanics, enabling them to tailor treatments and rehabilitation plans more effectively. This technological advancement is instrumental in improving the management of complex knee injuries, ensuring a more accurate diagnosis and effective treatment outcomes.
The Dyneelax arthrometer extends its capabilities beyond simple rotational analysis by measuring the Anteromedial (AM), Posterolateral (PL), Anterolateral (AL), and Posteromedial (PM) corners of the knee. This comprehensive analysis allows for a detailed evaluation of both the rotational and translational dynamics of the knee joint. This multifaceted approach provides a complete picture of knee joint stability, crucial for accurate diagnosis and effective treatment planning in complex knee injuries.
Building on the foundation laid by the introduction of the Dyneelax arthrometer for rotational stability analysis, a series of studies have further illuminated its importance. The 2014 study by Mouton et al. emphasized the importance of combining anterior and rotational laxity measurements to characterize knee laxity profiles in healthy individuals. This approach sheds light on the complex nature of knee laxity, underscoring the significance of rotational stability in assessing knee health. Subsequent studies have built upon this foundation. For example, the 2015 study by Mouton et al. further validated the combined measurement approach for a more comprehensive understanding of knee mechanics.
Furthermore, the 2016 study by Nicolas Ruiz explored the comparative role of the ACL and anterolateral structures in controlling passive internal rotation of the knee, highlighting the complexity of rotational dynamics in knee stability. Senioris’ 2017 study underlined the validity of assessing rotational laxity coupled with anterior translation, reinforcing the need for multifaceted measurement in knee diagnostics. Finally, the 2023 study by Théo Cojean evaluated the sensitivity, repeatability, and reproducibility of the Dyneelax, a newly developed knee arthrometer, providing essential insights into its clinical application. These studies collectively underscore the critical role of rotational stability analysis in understanding and diagnosing ACL injuries.
2.3 Future Developments: Artificial Intelligence (AI), Combined Translation and Rotation Analysis & Machine Learning (ML)
The future of dynamic knee testing is poised for transformative advancements with the integration of simultaneous translation and rotation analysis. This comprehensive approach will enable a more complete understanding of knee joint mechanics, particularly in the context of ACL injuries. By combining both translational and rotational data, clinicians will gain deeper insights into the complex interplay of forces at work within the knee joint.

Furthermore, another development that lies in the application of Artificial Intelligence (AI) and Machine Learning (ML) in this field is particularly promising. These technologies have the potential to revolutionize the way we interpret complex biomechanical data, allowing for more precise and personalized diagnostics and treatment plans. AI algorithms can analyze vast datasets, identifying patterns and correlations that might be missed by traditional analysis methods. Machine learning, on the other hand, can continually improve the accuracy and reliability of these assessments over time, learning from each case to enhance future diagnostics.
Enhancing the future of dynamic knee testing, the integration of Artificial Intelligence (AI) into this field opens up exciting possibilities. A study by Mouchotte et al. (2023) exemplifies this progression, showcasing the use of machine learning to interpret GNRB® knee arthrometer results for more accurate ACL injury diagnosis. This incorporation of AI with dynamic testing and MRI data represents a significant evolution in orthopedic diagnostics. It paves the way for more precise, non-invasive diagnostics, leveraging AI’s power to analyze complex data sets and improve clinical decision-making. This advancement signals a transformative era in knee injury management, where AI-driven insights contribute to enhanced patient care.
3. Integrating Dynamic Testing into Clinical Practice│Pre-Surgery Phase
In contemporary orthopedic practice, the treatment pathway for Anterior Cruciate Ligament (ACL) injuries typically begins with a clinical examination, followed by Magnetic Resonance Imaging (MRI) for confirmation, and, in cases of complete tears, culminates in ACL reconstruction surgery. Post-operative rehabilitation is then initiated to restore function and strength. This conventional approach, while effective, often overlooks the nuances of partial tears and dynamic instability.
The integration of dynamic knee testing using GNRB and Dyneelax arthrometers can significantly enhance this traditional treatment pathway. In the revised protocol, after the initial clinical examination, dynamic testing would be employed before or alongside MRI. This step is crucial for a more accurate assessment of the knee’s functional stability, particularly beneficial in detecting partial ACL ruptures that might not be evident in static MRI scans.
3.1 Treatment Pathway Integration
Integrating dynamic knee testing into the diagnostic pathway for ACL injuries requires thoughtful coordination with existing protocols. The process starts with a clinical examination, which typically involves a thorough patient history to understand the mechanism of injury and symptoms. Physical examinations, including the Lachman test, pivot shift test, and anterior drawer test, are performed to assess knee laxity and stability. These tests help in forming an initial hypothesis about the nature and extent of the injury.
Following the clinical assessment, dynamic testing using tools like the GNRB and Dyneelax arthrometers should be the next step. This advanced analysis offers an in-depth assessment of knee stability, particularly useful in cases where the clinical examination suggests potential partial ACL tears (Read Théo Cojean et al. in 2023) or complex injuries involving rotational instability (Read a second study, the same year by Théo Cojean). Dynamic testing provides quantifiable data on anterior/posterior tibial translation and medial/lateral rotation, offering a more nuanced understanding of the knee’s functional state than what can be discerned from manual tests alone.

If the results from dynamic testing indicate significant abnormalities, an MRI might be recommended for further evaluation and to visualize the soft tissue structures in detail. This step is particularly important in cases where the dynamic testing suggests severe injury or when the clinical picture is unclear.
The subsequent treatment plan is formulated based on the combined insights from the clinical examination, dynamic testing, and MRI findings. Treatment options can range from conservative management, like physiotherapy and bracing, to surgical interventions such as ACL reconstruction. The precise nature and extent of the injury, as interpreted from the various diagnostic modalities, guide the choice of treatment.
In this integrated pathway, each step serves a specific purpose, with dynamic testing positioned as a crucial intermediate step that enhances the diagnostic accuracy and aids in formulating a more tailored treatment approach. This sequence not only ensures a thorough evaluation of the knee injury but also contributes to more effective and patient-specific management strategies.
3.2 Cost-Effectiveness and Efficiency
Before beginning this section, please note that our example is based on the French Healthcare System, where a robotic arthrometer test costs around 65€. It’s important to emphasize that the arguments and insights discussed can be applied globally. In our experience, the cost for arthrometer tests conducted with our devices varies internationally, ranging from 20€ to 200€.
Dynamic testing acts as an initial filter in the diagnostic process. Considering the cost of an MRI (around €500 in average in France in the private sector), dynamic testing, which costs approximately €65, is a more economical initial step. This cost-effective approach could reserve MRI for cases where it’s absolutely necessary, reducing expenses for patients and the french healthcare system. Moreover, other pathologies that crucially depend on quick MRI access, such as tumors or spinal injuries, would benefit from reduced MRI wait times, which currently average 30 days in France (Snitem Data in 2017).
3.3 Advantages of Dynamic Testing
The primary advantage of including dynamic testing is the enhanced detection of partial ACL ruptures (Read Théo Cojean et al. in 2023) and a more comprehensive understanding of knee dynamics. This leads to more personalized treatment plans, potentially avoiding unnecessary surgeries or optimizing surgical outcomes by accurately assessing the knee’s condition. Additionally, dynamic testing provides valuable data for tailoring rehabilitation protocols (Read Nouveau et al. – 2017), potentially reducing recovery times and improving long-term joint stability (Read 2023 study by Forelli et al. ).
3.4 Administrative and Practical Considerations
Clinics must consider the practical aspects of incorporating dynamic testing, including scheduling efficiency to avoid diagnostic delays. Moreover, navigating insurance and billing implications is crucial to ensure patient accessibility to these advanced diagnostics.
To summerize, integrating dynamic knee testing into clinical practice presents a forward-thinking approach in ACL injury management. It offers a more nuanced diagnostic capability, leading to more precise treatment decisions and potentially better patient outcomes. This integration, however, requires careful planning in terms of equipment procurement, staff training, procedural adjustments, and administrative handling, ensuring a smooth transition to this advanced diagnostic approach.
4. Integrating Dynamic Testing into Rehabilitation│Post-Surgery Phase
4.1 Objective Measurement and Monitoring

These devices offer detailed data on knee laxity and compliance throughout the rehabilitation process. A 2016 study by Semay et al. highlighted the evolution of anteroposterior laxity at various post-surgical stages, demonstrating the importance of continuous monitoring.
Similarly, the 2019 study by Pouderoux et al. noted changes in joint laxity and graft compliance during the first postoperative year, emphasizing the need for ongoing assessment to track the healing progress.
4.2 Tailored Rehabilitation Programs
The use of robotic arthrometers in post-surgery rehabilitation facilitates the development of tailored rehabilitation programs (Click here to see Rehab Programs using arthrometers), which are crucial for optimal recovery. By closely monitoring the knee’s recovery trajectory, these devices enable clinicians to design rehabilitation protocols that cater to the individual needs and progress of each patient.
The 2017 study by Nouveau-Robert-Viel provides valuable insights into this aspect. It examined how early mechanical solicitations of the knee influence the final stiffness of the ACL graft post-surgery. This study underscores the importance of customizing the rehabilitation process based on how the graft responds at different stages of healing. For instance, a graft that exhibits greater laxity or compliance in the early stages of rehabilitation may require a more conservative approach, with gradual progression in the intensity and range of exercises.
Furthermore, robotic arthrometers can help in determining the appropriate timing for introducing different types of exercises and activities. This is particularly important to avoid overloading the graft before it has sufficiently healed, which can compromise the graft’s integrity and potentially lead to reinjury.
In addition to guiding exercise intensity and progression, these detailed measurements also aid in other aspects of rehabilitation, such as proprioceptive training and neuromuscular control. This holistic approach ensures not only the physical healing of the graft but also the restoration of functional stability and movement patterns, which are critical for a safe return to sports and daily activities.
The ability to tailor rehabilitation programs based on objective data from robotic arthrometers aligns with the evolving trend in medicine towards personalized care. It acknowledges that each patient’s path to recovery is unique, and their rehabilitation should be adjusted accordingly. This patient-specific approach maximizes the effectiveness of rehabilitation, ultimately leading to better outcomes and a higher likelihood of a successful return to pre-injury levels of activity.
4.3 Enhanced Patient Engagement and Motivation
Seeing objective data can significantly boost patient morale and adherence to rehabilitation plans. This aspect was touched upon in the 2023 study by Forelli, which discussed various post-operative rehabilitation strategies, including the role of patient engagement in recovery.
4.4 Reducing the Risk of Reinjury
Accurate assessment through robotic arthrometers aids in identifying potential risks of reinjury. By understanding the specific weaknesses in a patient’s knee stability, clinicians can adjust treatment plans to mitigate these risks, a concept further explored in the studies mentioned above.
4.5 Cost-Effectiveness in the Long Term
While the initial investment in such technology may be substantial, the benefits of optimized rehabilitation and reduced reinjury risks can lead to long-term cost savings. This was reflected in the broader implications of the studies by Semay et al. and Pouderoux et al., where efficient rehabilitation had implications for overall healthcare costs related to ACL injuries.
In summary, robotic arthrometers play a vital role in post-surgery rehabilitation, providing valuable insights into knee recovery and aiding in the development of personalized rehabilitation plans. Their use is supported by various studies that highlight the importance of continuous and precise monitoring of the knee’s healing process.
5. Challenges and Limitations
Adopting dynamic testing in clinical settings presents certain challenges and limitations that must be acknowledged and addressed. One of the primary concerns is the cost of equipment. Advanced robotic arthrometers like the GNRB and Dyneelax represent significant financial investments, which might be prohibitive for some healthcare facilities, especially those with limited budgets.

Another challenge lies in the training and expertise required to effectively use these advanced systems. Ensuring that medical professionals are proficient in operating these devices and interpreting their data requires time and resources. There is also the need to integrate dynamic testing into existing diagnostic workflows, which may involve overcoming resistance to change and adjusting long-established clinical protocols.
In terms of limitations, while dynamic testing provides enhanced diagnostic capabilities, it should not be viewed as a standalone solution. It is most effective when used in conjunction with other diagnostic tools, like MRI, necessitating a balanced approach to patient assessment.
Future research and development in this field should focus on making dynamic testing more accessible and user-friendly. Efforts could include reducing the cost of these systems, developing more intuitive interfaces, and creating comprehensive training programs. Additionally, research should aim to further validate the effectiveness of dynamic testing in various clinical scenarios, expanding its applicability and integrating it more seamlessly into diverse healthcare settings.
Conclusion
The integration of dynamic testing in the diagnosis and treatment of Anterior Cruciate Ligament (ACL) injuries marks a significant advancement in orthopedic and sports medicine. The use of advanced robotic arthrometers like the GNRB and Dyneelax has revolutionized our approach to understanding knee joint mechanics, particularly in the context of complex ACL injuries.
Dynamic testing offers a more nuanced assessment than traditional methods, especially in detecting partial ACL ruptures and assessing rotational instabilities. Its ability to provide objective, quantifiable data on knee stability is invaluable in formulating precise and personalized treatment plans. This technology enhances the diagnostic process, bridging the gap between initial clinical examinations and static imaging methods like MRI.
In post-surgery rehabilitation, these tools play a crucial role in monitoring recovery and guiding rehabilitation protocols. By offering detailed insights into the knee’s functional recovery, they enable tailored rehabilitation programs, leading to more effective patient outcomes and a reduced risk of reinjury.
However, the adoption of dynamic testing is not without its challenges. The cost of equipment and the need for specialized training are significant barriers. Additionally, integrating these advanced diagnostics into existing clinical workflows requires careful consideration and adaptation.
Looking forward, the potential of dynamic testing in ACL injury management is vast. Future research should focus on enhancing accessibility, further validating its effectiveness, and exploring the integration of Artificial Intelligence and Machine Learning for even more sophisticated diagnostics.
In conclusion, dynamic testing represents a transformative approach in the management of ACL injuries. Its integration into clinical practice promises a future where diagnostics are more precise, rehabilitation is more personalized, and patient outcomes are significantly improved. As we continue to embrace and refine this technology, it stands to greatly benefit patients and healthcare providers alike in the realm of orthopedic care.
Medical References
- Cojean, T., Batailler, C., Robert, H., Cheze, L. (2023). GNRB® laximeter with magnetic resonance imaging in clinical practice for complete and partial anterior cruciate ligament tears detection: A prospective diagnostic study with arthroscopic validation on 214 patients. The Knee, 42, 373-381. DOI: 10.1016/j.knee.2023.03.017
- Nouveau, S., Robert, H., Viel, T. (2017). ACL Grafts Compliance During Time: Influence of Early Solicitations on the Final Stiffness of the Graft after Surgery. J Orthop Res Physiother, 3(1) DOI: 10.24966/ORP-2052/100035
- Pouderoux, T., et al. (2019). Joint laxity and graft compliance increase during the first year after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. DOI: 10.1007/s00167-019-05711-z
- Forelli, F., et al. (2023). After surgery rehab post op 2023. J Orthop Sports Phys Ther, 48(10), 801-811. DOI: 10.26603/001c.73031.
- Mouton, C., Seil, R., Meyer, T., Agostinis, H., Theisen, D. (2014). Combined anterior and rotational laxity measurements allow characterizing personal knee laxity profiles in healthy individuals. Knee Surg Sports Traumatol Arthrosc. DOI: 10.1007/s00167-014-3244-6.
- Mouton, C., Theisen, D., Meyer, T., Agostinis, H., Nührenbörger, C., Pape, D., Seil, R. (2015). Combined anterior and rotational knee laxity measurements improve the diagnosis of anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc, 23(8), 2859-2867. DOI: 10.1007/s00167-015-3757-7.
- Ruiz, N., Filippi, G. J., Gagnière, B., Bowen, M., Robert, H. E. (2016). The Comparative Role of the Anterior Cruciate Ligament and Anterolateral Structures in Controlling Passive Internal Rotation of the Knee: A Biomechanical Study. DOI: 10.1016/j.arthro.2016.02.017.
- Senioris, A., et al. (2017). Validity of rotational laxity coupled with anterior translation of the knee: A cadaveric study comparing radiostereometry and the Rotab®. DOI: 10.1016/j.knee.2017.01.009.
- Cojean, T., Batailler, C., Robert, H., Cheze, L. (2023). Sensitivity, repeatability and reproducibility study with a leg prototype of a recently developed knee arthrometer Dyneelax. Medicine in Novel Technology and Devices, 19. DOI: 10.1016/j.medntd.2023.100254.
- Klouche, S., Lefevre, N., Cascua, S., Herman, S., Gerometta, A., Bohu, Y. (2015). Diagnostic value of the GNRB® in relation to pressure load for complete ACL tears: A prospective case-control study of 118 subjects. Orthopaedics & Traumatology: Surgery & Research, 101(3), 297-300. DOI: 10.1016/j.otsr.2015.01.008.
- Jenny, J.-Y., Puliero, B., Schockmel, G., Harnoist, S., Clavert, P. (2017). Experimental validation of the GNRB® for measuring anterior tibial translation. OTSR. DOI: 10.1016/j.otsr.2016.12.011.
- Smith, K., Miller, N., Laslovich, S. (2022). The Reliability of the GNRB® Knee Arthrometer in Measuring ACL Stiffness and Laxity: Implications for Clinical Use and Clinical Trial Design. IJSPT, 17(6), 1016-1025. DOI: 10.26603/001c.38252.
- Magdič, M., Dahmane, R. G., Vauhnik, R. (2023). Intra-rater reliability of the knee arthrometer GNRB® for measuring knee anterior laxity in healthy active subjects. Journal of Orthopaedics, 39, 7-10. DOI: 10.1016/j.jor.2023.03.016.
- Semay, B., Rambaud, A., Philippot, R. (2016). Evolution of the anteroposterior laxity by GnRB at 6, 9, and 12 months post-surgical anterior cruciate ligament reconstruction. DOI: 10.1016/j.rehab.2016.07.045
- Mouchotte, J., LeBerre, M., Cojean, T., Robert, H. (2023). New interpretation of GNRB® knee arthrometer results for ACL injury diagnosis support using machine learning. Machine Learning with Applications, 13, 100480. DOI: 10.1016/j.mlwa.2023.100480