Anterior Cruciate Ligament (ACL)reconstruction is a cornerstone in the management of knee instability, playing a pivotal role in mitigating the risk of long-term degenerative changes. The ACL is crucial for maintaining knee stability, especially in athletes and individuals engaged in high-demand activities. Injuries to this ligament can lead to significant functional impairment, necessitating surgical intervention to restore stability and prevent the progression to osteoarthritis.
Over the years, the evolution of ACL tunnel surgery techniques has markedly influenced the outcomes of ACL reconstruction. From the traditional transtibial method to more anatomically faithful approaches like the anteromedial portal technique, each evolution has sought to better mimic the natural anatomy and biomechanics of the ACL. These advancements have been driven by a deeper understanding of the knee’s kinematics, leading to improved patient outcomes, reduced recovery times, and a lower incidence of post-surgical complications.
In parallel, the integration of dynamic arthrometry into the preoperative planning phase has emerged as a game-changer. The DYNEELAX® system, a cutting-edge example of this technology, offers surgeons a nuanced view of the knee’s biomechanical behavior under dynamic conditions. By measuring antero-posterior tibial translation and internal/external tibial rotation, the DYNEELAX® provides critical data that can guide the surgeon in selecting the most appropriate tunnel surgery technique. This personalized approach ensures that the surgical intervention is finely tailored to the individual patient’s anatomy and biomechanical deficiencies, significantly enhancing the potential for optimal outcomes.
The promise of personalized surgical planning, augmented by tools like the DYNEELAX®, represents a leap forward in ACL reconstruction. It not only underscores the importance of precision in surgical technique but also highlights the potential for technology to refine and enhance the surgeon’s ability to restore knee stability and function.
I. The Anatomy of ACL Reconstruction

The Anterior Cruciate Ligament (ACL) is one of the key ligaments that stabilize the knee joint, connecting the femur (thigh bone) to the tibia (shin bone). It plays a crucial role in preventing the tibia from sliding out in front of the femur, as well as providing rotational stability to the knee. This is essential not just for high-performance athletics but also for everyday activities that involve knee flexion and extension.
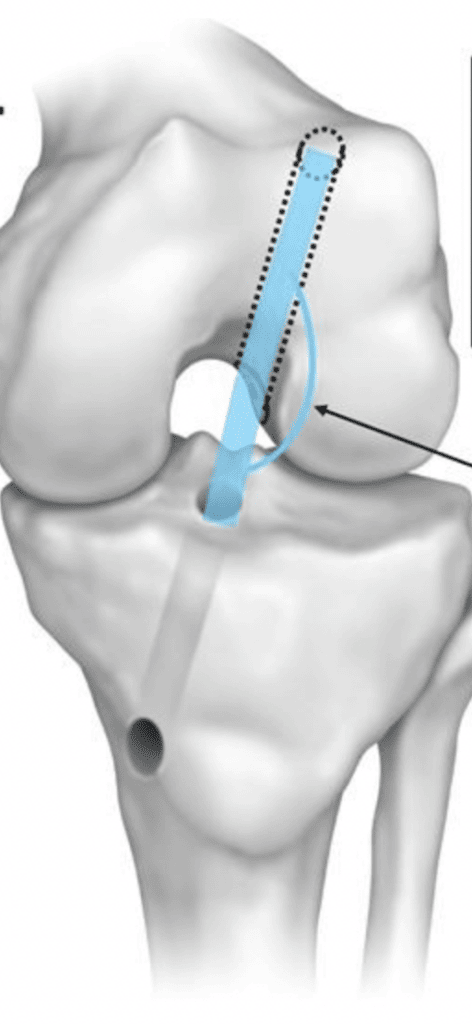
Biomechanically, the ACL is composed of two main bundles, the anteromedial (AM) and posterolateral (PL), each with distinct roles depending on the knee’s position. During knee movement, these bundles work synergistically to control kinematics, with the AM bundle primarily resisting anterior tibial translation and the PL bundle contributing to rotational stability and proprioception. This complex interplay is critical for maintaining knee stability and function.
The pathophysiology of ACL injuries often involves a combination of excessive force and motion that exceeds the ligament’s tensile strength, typically during activities that involve sudden stops, changes in direction, or direct impact. These injuries can lead to knee instability, changes in gait, and an increased risk of secondary knee injuries and osteoarthritis if not properly addressed.
ACL reconstruction aims to restore the knee’s stability and function by replicating the native ACL’s anatomy and kinematics as closely as possible. The procedure involves replacing the torn ligament with a graft, which can be autograft (taken from the patient’s own body), allograft (donor tissue), or synthetic substitutes. The goal is to recreate the ligament’s original biomechanical properties, thereby restoring the normal kinematic behaviour of the knee joint. This involves precise placement of the graft in tunnels drilled in the femur and tibia at the anatomical insertion points of the native ACL, ensuring the new ligament can withstand the mechanical forces exerted during physical activities and effectively stabilize the knee. Successful ACL reconstruction allows patients to return to their pre-injury levels of activity while minimizing the risk of future injuries and degenerative changes.
II. ACL Tunnel Surgery Techniques
2.1 Transtibial Technique (TT)
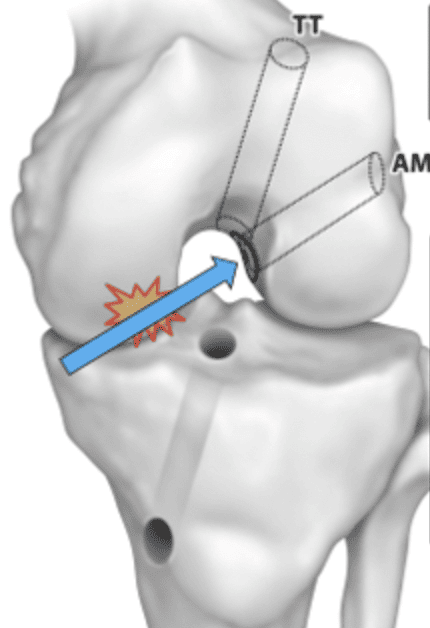
The transtibial technique (TT) in ACL reconstruction is a traditional approach where the femoral tunnel is drilled through the tibial tunnel. This method has been widely utilized due to its simplicity and effectiveness in restoring knee stability. The procedural steps involve creating a tunnel in the tibia, which is then used as a guide to drill the femoral tunnel. This technique aims to place the graft in a position that replicates the original ACL’s biomechanical function, focusing on restoring anterior-posterior stability of the knee.
Advantages of the transtibial technique include its straightforward procedural steps and the relatively short learning curve for surgeons. It allows for effective restoration of knee stability in many patients, making it a reliable choice for ACL reconstruction.
However, limitations exist, particularly concerning the anatomical accuracy of tunnel placement. The transtibial approach may result in less optimal positioning of the femoral tunnel, potentially leading to a more vertical graft orientation. This orientation might not perfectly replicate the native ACL’s anatomy, which can affect the knee’s rotational stability and overall biomechanical function. Studies like the one from Silva et al. – 2012 have indicated that while the transtibial technique is effective in many cases, alternative methods like the anteromedial portal technique may offer better outcomes in terms of anatomical placement and knee stability.
The choice between the transtibial and other techniques depends on various factors, including the surgeon’s expertise, the specific anatomy and biomechanics of the patient’s knee, and the desired outcomes. While the transtibial technique has been a staple in ACL reconstruction, evolving techniques and continuous research are essential to optimize surgical outcomes and patient satisfaction.
- Approach: The femoral tunnel is drilled through the tibial tunnel, which historically was the standard technique, allowing for a straightforward surgical procedure.
- Graft Placement: This technique often results in a more vertical orientation of the ACL graft, which may not replicate the natural anatomy as closely as other methods.
- Visibility and Access: Direct visualization of the femoral tunnel placement is more challenging, potentially affecting the anatomical accuracy of the graft placement.
- Advantages:
- Simplicity and familiarity of the technique for many surgeons.
- Requires standard surgical instruments and equipment.
- Generally quicker surgical times due to the straightforward approach.
- Disadvantages:
- Risk of non-anatomical graft placement, potentially affecting knee biomechanics and stability.
- Increased risk of impingement and graft wear over time.
- Less optimal outcomes in terms of rotational stability.
- Technical Considerations:
- Surgeons must carefully plan the tibial tunnel placement to optimize femoral tunnel alignment.
- Modifications of the technique may be necessary to achieve more anatomical graft placement.
- Attention to the angle of drilling and knee flexion during tunnel creation is important.
2.2 Anteromedial Portal Technique (AM)
The anteromedial portal technique represents a significant advancement in achieving anatomical accuracy in femoral tunnel placement. Unlike the transtibial approach, this technique allows the surgeon to drill the femoral tunnel independently of the tibial tunnel, providing enhanced flexibility in positioning. This procedural nuance is instrumental in placing the graft in a more anatomically correct position, closely mimicking the native ACL’s insertion points.
Benefits of the anteromedial portal technique are notable, particularly regarding anatomical placement and rotational stability. By facilitating a more accurate replication of the ACL’s natural anatomy, this method offers improved outcomes in terms of knee kinematics and stability. Comparative studies have supported these advantages, showing that the anteromedial portal approach can lead to better rotational control and overall knee function post-reconstruction (Read Silva et al. – 2012 for more info). Specifically, the technique has been linked with more centrally placed femoral and tibial tunnels within the ACL footprint compared to the transtibial method, as highlighted in clinical trials and systematic reviews.
However, the technique is not without its potential complications and a steep learning curve. Surgeons may face challenges related to the precise creation of the anteromedial portal and the risk of damaging surrounding structures due to the intricate nature of tunnel placement. Moreover, mastering this approach requires a thorough understanding of knee anatomy and proficient arthroscopic skills, as evidenced by research indicating a gradual improvement in outcomes as surgeons gain experience with this technique.
While the anteromedial portal technique offers significant advantages in terms of anatomical accuracy and potential for improved patient outcomes, it demands a higher level of surgical expertise. PubMed studies, such as those comparing it directly with the transtibial approach, provide a valuable resource for surgeons looking to evaluate the benefits and challenges associated with this advanced ACL reconstruction method (Read Silva et al. – 2012 for more info).
- Approach: Uses a separate, more anteriorly and medially created portal for femoral tunnel drilling, aiming for an anatomical graft placement with a more horizontal orientation.
- Graft Placement: Allows for a horizontal femoral tunnel orientation, which can help restore the knee’s rotational stability and closely replicate the ACL’s natural function.
- Visibility and Access: Provides good visibility of the femoral ACL attachment site, though the surgical angle can be more challenging compared to the transportal technique.
- Advantages:
- Horizontal tunnel placement potentially offers better rotational stability.
- Reduced risk of damaging the medial femoral condyle.
- May lead to better outcomes in knee stability and patient satisfaction.
- Disadvantages:
- Technical challenges in achieving correct tunnel angle without compromising structures.
- Risk of too anterior a tunnel, affecting graft tension and biomechanics.
- Limited visibility may require greater reliance on experience and instrumentation.
- Technical Considerations:
- Accurate determination of the entry point for the femoral tunnel is crucial.
- Flexible reamers or specialized guides can assist in achieving desired tunnel positions.
- The knee’s flexion angle during drilling is vital for anatomic graft placement.
2.3 Outside-In Technique (OI)
The Outside-In (OI) technique for ACL reconstruction is recognized for its precision in femoral and tibial tunnel placement, closely mirroring the native ACL’s footprint. This approach facilitates the placement of the graft in a position that optimally replicates the ligament’s natural orientation and tensioning, which is crucial for the knee’s biomechanical function. A study highlighted that the OI technique allowed for the femoral tunnel to be placed in a position that is low, oblique, and posterior on the femoral side, effectively mimicking the native ACL, which is essential for achieving the desired biomechanical outcomes (Read Sinha et al. – 2014).
Compared to the transtibial and anteromedial portal techniques, the OI method offers distinct advantages in terms of surgical precision and the ability to customize tunnel placement according to the patient’s anatomy. This is particularly beneficial in complex cases or revision surgeries, where anatomical variances or previous surgical alterations need to be considered. The technique has been shown to be reproducible and simple, with a significant improvement in patients’ Lysholm scores post-surgery and the maintenance of full range of motion (Read Sinha et al. – 2014).
However, studies comparing the OI technique with the anteromedial (AM) portal approach have found no significant differences in clinical outcomes, including graft healing, knee stability, and return to pre-operative levels of activity, by two years post-operation (Read CarlLee et al. – 2017). This suggests that while the OI technique may offer specific advantages in tunnel placement and potentially in revision scenarios, the choice between OI and AM techniques may ultimately depend on the surgeon’s preference, the patient’s specific anatomy, and the clinical context.
The learning curve and potential for complications, while not as pronounced as with other methods, still necessitate a thorough understanding of knee anatomy and proficiency in arthroscopic surgery to minimize risks and maximize the benefits of the OI technique.
The Outside-In technique stands out for its precision in tunnel placement and flexibility, making it a valuable option for ACL reconstruction, especially in challenging cases. Its effectiveness, as demonstrated through improvements in patient scores and maintenance of knee function, underlines its role in the arsenal of ACL reconstruction techniques.
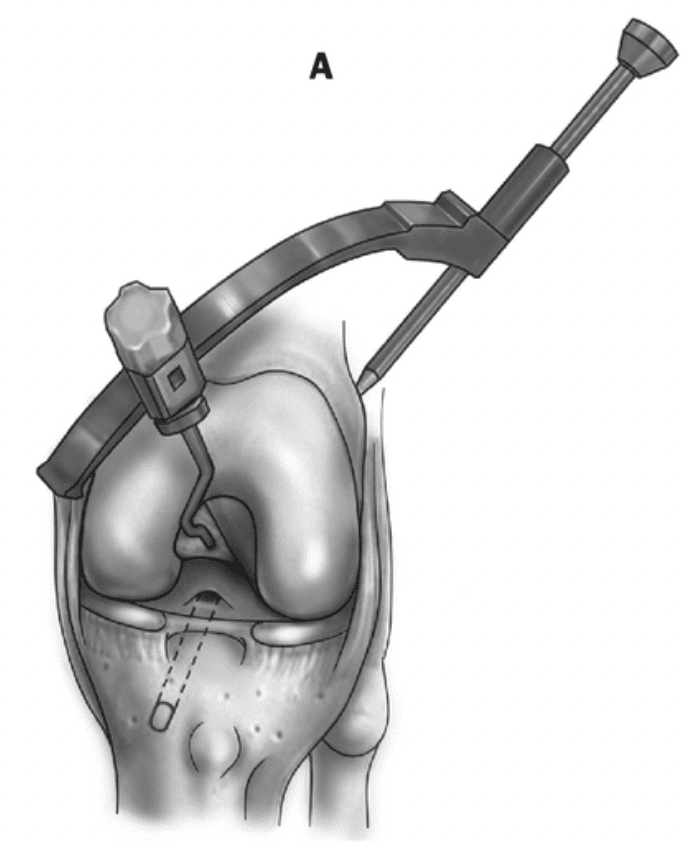
- Approach: Involves drilling the femoral tunnel from the lateral thigh to the inside of the knee, allowing for controlled placement of the femoral tunnel independent of the tibial tunnel.
- Graft Placement: Offers flexibility in graft placement, enabling a more anatomical reconstruction of the ACL with potentially better control over tunnel orientation.
- Visibility and Access: Provides good control and visualization of the femoral tunnel placement, facilitating an anatomical approach.
- Advantages:
- Anatomical graft placement enhances knee stability and biomechanics.
- Reduced risk of damaging intra-articular structures during femoral tunnel creation.
- Allows for precise control over the femoral tunnel angle and position.
- Disadvantages:
- Potentially more invasive with a higher risk of soft tissue damage due to the outside-in drilling.
- Requires careful planning and surgical skill to optimize tunnel placement and avoid complications.
- May involve longer surgical times compared to some other techniques.
- Technical Considerations:
- Accurate determination of femoral tunnel entry and exit points is crucial.
- Surgeons must manage soft tissue carefully to prevent complications.
- Flexibility in tunnel placement allows for customized graft positioning based on patient anatomy.
2.4 Over-the-Top Technique (OTT)
The Over-the-Top (OTT) technique for ACL reconstruction is a less invasive approach with a rich historical context, initially popularized for its simplicity and effectiveness in treating ACL injuries without the need for drilling through the bone. This technique involves passing the graft over the top of the femoral condyle to reconstruct the ACL, thereby avoiding the risks associated with tunnel drilling. It has seen a resurgence in specific clinical scenarios, particularly for skeletally immature patients and in revision surgeries where traditional tunnel drilling might pose additional risks or complications.
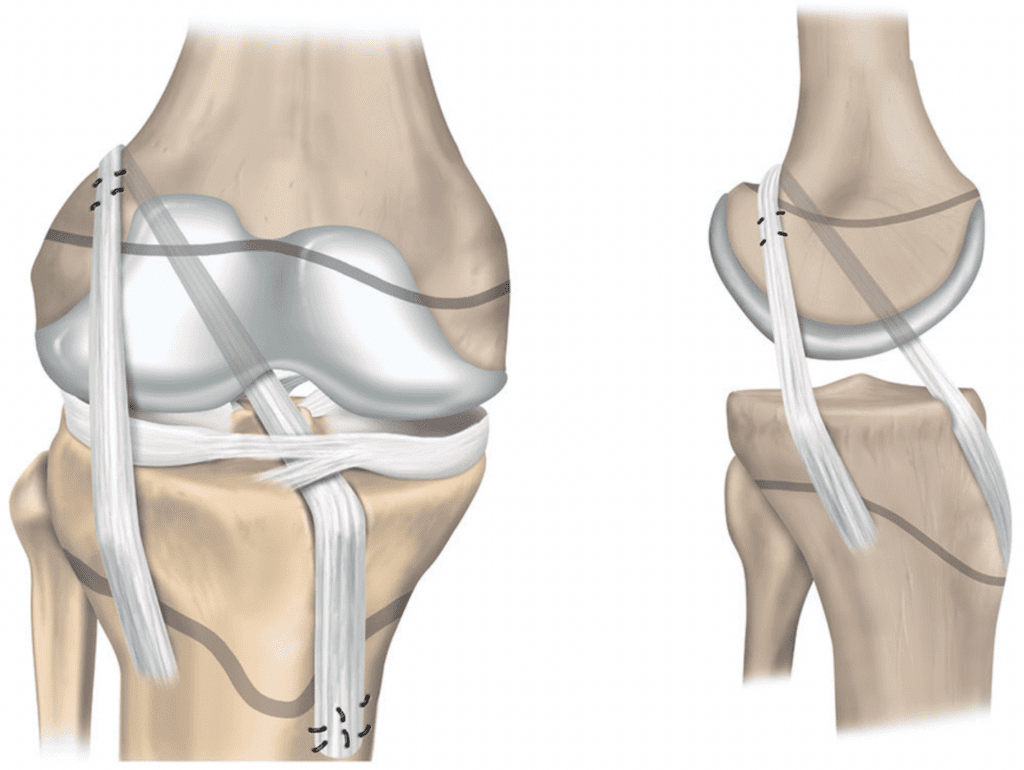
Current applications of the OTT technique are especially beneficial in skeletally immature individuals and revision settings, where preserving bone stock and avoiding growth plate damage are crucial considerations. It has been shown to effectively restore anterior and rotatory knee laxity, offering a reliable option in these complex cases. The technique is praised for its wide application, simple operation, and quick recovery, making it an attractive choice for primary and revision ACL reconstructions (Reference Study: Nagai et al. – 2020 & Mei et al. – 2022).
Evidence suggests that outcomes related to stability and function with the OTT technique are comparable to those achieved with more traditional approaches, such as all-inside, transtibial, and anteromedial portal drilling techniques. This includes revision settings where maintaining knee stability and function is paramount. Despite its non-anatomic nature, the OTT approach has been associated with good mid-term outcomes, low rates of residual rotatory laxity, complications, and failures, underscoring its viability as a surgical option (Reference Study: Sarraj et al. – 2019).
Moreover, a biomechanical evaluation highlighted the OTT technique’s potential in providing enhanced rotational stability compared to conventional single-bundle ACL reconstruction, particularly at lower flexion angles. This suggests biomechanical superiority in certain aspects, which could translate to clinical advantages in primary and revision ACL reconstruction scenarios (Reference Study: Min et al. – 2022).
The Over-the-Top technique stands as a viable, less invasive option for ACL reconstruction, particularly suited for skeletally immature patients and revision cases. Its ability to restore knee stability and function, combined with a simple operative approach and quick recovery, makes it an important tool in the orthopedic surgeon’s repertoire. Further research is anticipated to optimize graft selection and management of the femoral condyle to enhance long-term outcomes.
- Approach: Avoids drilling a femoral tunnel by passing the graft over the top of the lateral femoral condyle, simulating the natural course of the ACL.
- Graft Placement: Can achieve an anatomical replication of the ACL’s course without the need for femoral bone drilling, potentially preserving bone stock.
- Visibility and Access: The technique relies on careful surgical planning and skill to position the graft correctly without direct visualization of the femoral attachment.
- Advantages:
- Preserves femoral bone stock, which is beneficial in revision surgeries or pediatric cases.
- Reduced risk of damaging critical structures around the femur.
- May be less technically demanding in terms of drilling precision.
- Disadvantages:
- Risk of non-anatomical graft tensioning and placement.
- Potential for increased graft mobility and wear due to the lack of bone tunnel fixation.
- Challenges in securing the graft and achieving optimal tension.
- Technical Considerations:
- Precise graft preparation and fixation techniques are essential to ensure stability.
- Surgeons must be experienced in soft tissue management and graft tensioning.
- Suitable mostly for specific patient populations or in conjunction with other techniques.
2.5 All-Inside Technique
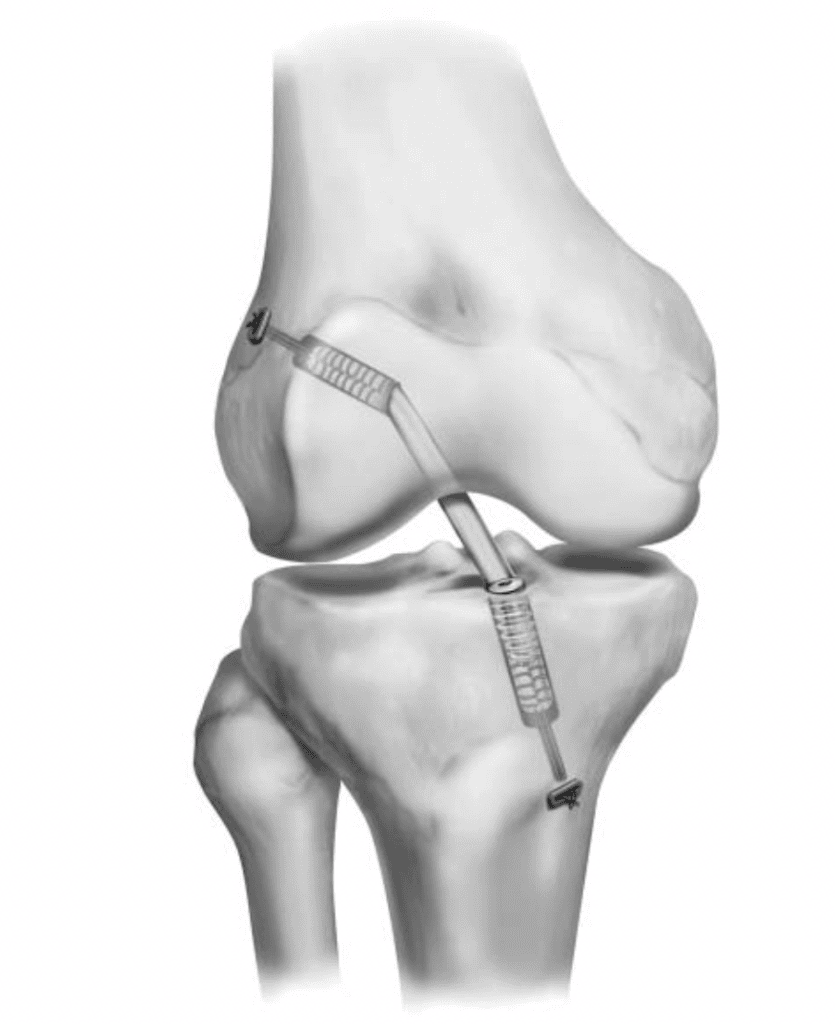
The All-Inside Technique for Anterior Cruciate Ligament (ACL) Reconstruction is an innovative, minimally invasive approach that aims to improve patient outcomes by reducing surgical invasiveness, minimizing pain, and enabling faster recovery.
Unlike traditional methods that create full bone tunnels, the all-inside technique utilizes bone sockets for ACL graft passage and typically employs suspensory fixation instead of screw fixation to secure the graft. This technique can be applied using various graft types, including all soft tissue, bone plug ACL grafts, autograft hamstring, or quadriceps tendon, and most allograft tendon options (Reference Study: Nuelle et al. – 2022).
Advantages of the all-inside technique include anatomical tunnel/socket placement, decreased postoperative pain and swelling, minimal hardware, effective graft tensioning and retensioning, and circumferential graft to bone healing. Matching graft diameter to socket diameter and drilling appropriate length sockets based on individual graft length are crucial for avoiding complications such as graft-socket mismatch, full-tunnel reaming, and loss of cortical fixation (Reference Study: Nuelle et al. – 2022).
Graft Selection and Fixation: The technique allows for the use of various graft types, with the preparation involving duplication and quadrupling of the graft, secured with high-strength multi-strand sutures. This preparation ensures the graft is robust and ready for implantation (Reference Study: Bosco et al. – 2023).
Clinical Outcomes: Studies have shown significant improvements in functional outcomes, such as the International Knee Documentation Committee score, Lysholm score, visual analog scale score, and Tegner activity score, from baseline to final follow-up, with a majority of patients returning to their pre-injury levels of activity. The technique has been associated with similar or superior biomechanical properties and clinical outcomes compared to traditional full-tunnel ACL reconstruction techniques, though concerns regarding higher graft failure rates have been noted (Reference Studies: Connaughton et al. – 2017 & Schurz et al. – 2016).
The all-inside ACL reconstruction technique offers a less invasive alternative with potential benefits including reduced postoperative pain, quicker recovery, and good functional outcomes. However, careful consideration of graft selection, meticulous surgical technique, and monitoring for possible higher graft failure rates are essential for optimizing patient outcomes. This approach underscores a significant advancement in ACL surgery, catering to the needs of patients and surgeons alike for effective, minimally invasive treatment options.
- Approach: Utilizes small incisions and specialized instruments to create sockets instead of full tunnels for the graft, minimizing bone removal and potentially reducing post-operative pain.
- Graft Placement: Allows for anatomical placement of the graft with less disruption to the knee’s anatomy, aiming to replicate the ACL’s natural orientation and function closely.
- Visibility and Access: Enhanced by the use of flexible instruments and arthroscopic visualization, facilitating precise graft placement.
- Advantages:
- Reduced trauma to the knee structure due to smaller incisions and less bone removal.
- Potentially quicker recovery and reduced post-operative pain.
- Improved cosmetic outcome with smaller scars.
- Disadvantages:
- Requires specialized instruments and higher surgical skill.
- May have limitations in graft selection and fixation options.
- Could have a higher cost due to the use of specialized equipment.
- Technical Considerations:
- Precision in tunnel placement is crucial to avoid complications.
- Surgeons must be adept at arthroscopic techniques and the use of flexible instruments.
- Careful attention to graft tensioning and fixation to ensure stability.
2.6 Transportal Technique (TP)
The TransPortal (TP) Technique for Anterior Cruciate Ligament (ACL) Reconstruction is a method that emphasizes anatomical graft placement to optimize the biomechanical restoration of the knee. This technique uses the anteromedial portal for drilling the femoral tunnel, which allows for more precise and anatomical placement of the ACL graft compared to the traditional transtibial (TT) approach.
The TP technique has been shown to achieve better clinical outcomes than the TT technique, particularly in terms of knee functional outcome scales and knee laxity tests, suggesting it may be a superior option for single-bundle ACL reconstruction (Reference Study: Ro et al. – 2018)
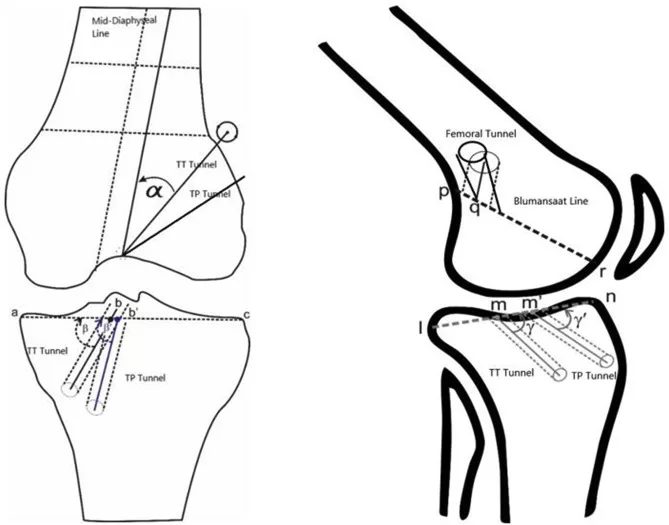
A notable advantage of the TP technique is its ability to produce improved positions in both the femoral and tibial tunnels. This is crucial for mimicking the native ACL’s anatomy as closely as possible, which in turn influences postoperative knee stability and reduces the potential for graft impingement. A study comparing tunnel positions found that the TP technique achieved more anatomically accurate positions, with none of the outliers that were present in the TT group, indicating a higher precision in graft placement (Reference Study: Yau et al. – 2013).
The TP approach has also been associated with better clinical and functional outcomes. For instance, patients who underwent ACL reconstruction using the TP technique showed significant improvements in various outcome measures, including the International Knee Documentation Committee score, Lysholm score, and visual analog scale score, from baseline to final follow-up. These improvements underscore the technique’s efficacy in restoring knee function and stability (Reference Study: Logan et al. – 2012).
Furthermore, the TP technique facilitates the anatomic placement of the femoral tunnel without the need for an accessory medial portal or hyperflexion of the knee, simplifying the surgical process while ensuring accuracy in graft placement. This direct measurement and drilling method through the lateral portal, viewing via the medial portal, enhance the procedure’s efficacy and minimize the technical challenges often associated with the anteromedial portal technique (Reference Study: Logan et al. – 2012).
The TransPortal ACL reconstruction technique offers a minimally invasive option with significant advantages in anatomical graft placement, leading to improved postoperative stability and function. Its emphasis on precision and anatomical fidelity makes it an appealing choice for ACL reconstructions, potentially offering better outcomes and reduced complications compared to traditional methods.
- Approach: Involves creating the femoral tunnel directly through the anteromedial portal, allowing for an anatomical placement of the ACL graft in the native footprint.
- Graft Placement: This method facilitates a more vertical orientation of the femoral tunnel, closely mimicking the ACL’s natural anatomy for potentially improved rotational stability.
- Visibility and Access: Offers excellent visibility and access to the femoral footprint, enabling precise tunnel placement with direct visualization.
- Advantages:
- Anatomical graft placement enhances knee stability.
- Vertical graft orientation may improve rotational stability.
- Direct visualization aids in accurate tunnel placement.
- Disadvantages:
- Higher surgical skill requirement and risk of complications, such as tunnel misalignment.
- Possible risk of neurovascular injury due to the proximity of critical structures.
- Steep angle drilling may lead to graft-tunnel mismatch or impingement.
- Technical Considerations:
- Precise portal placement and knee flexion angle management are critical.
- Specialized instruments may be necessary for navigating tight angles.
- Attention to avoiding damage to cartilage and knee structures is paramount.
III. Dynamic Arthrometry with Dyneelax: Enhancing Surgical Precision

The DYNEELAX® system represents a cutting-edge advancement in dynamic arthrometry, offering orthopedic surgeons a sophisticated tool for assessing knee stability. This system is designed to measure both Antero Posterior tibial Translation (APT) and Internal/External Tibial Rotation, providing a comprehensive analysis of knee mechanics. By quantitatively measuring these parameters, DYNEELAX® provides insights into the dynamic function of the knee, which are critical for planning ACL reconstruction surgeries (Study Reference: Cojean et al. – 2023)
The application of dynamic arthrometry data from the DYNEELAX® system can significantly influence the choice of tunnel surgery technique. For instance, a patient exhibiting more pronounced anterior-posterior tibial translation might benefit more from a technique that emphasizes the restoration of translational stability, such as the anteromedial portal or outside-in technique. Conversely, if the DYNEELAX® system identifies a significant internal/external tibial rotation instability, the surgical approach may lean towards techniques that offer better rotational stability correction, such as the over-the-top technique for example.
Adding to this, the results provided by the DYNEELAX® system may also guide the incorporation of additional surgical interventions such as the Lateral Extra-Articular Tenodesis (LET), the Lemaire technique, or extra-articular plasty. These techniques are considered when significant rotational instability is detected, which might not be fully addressed by standard ACL reconstruction alone. The LET technique, for instance, complements the intra-articular ACL reconstruction by providing additional support to control rotational movements, thereby enhancing the overall stability of the knee.
Evaluating the knee’s translation and rotation objectively, through detailed graphs and displacement/degrees metrics provided by DYNEELAX®, allows surgeons to tailor their surgical approach more precisely. By understanding the specific biomechanical deficiencies of a patient’s knee, surgeons can select a tunnel surgery technique that directly addresses the predominant mode of instability—be it translational or rotational. This decision-making process is enhanced by the Dyneelax system’s ability to provide real-time, dynamic assessments that reflect the knee’s behavior under physiological loads, rather than static measurements alone.
In essence, the DYNEELAX® system’s integration into ACL reconstruction planning embodies the shift towards personalized medicine. It enables a more tailored approach to surgery, potentially improving outcomes by ensuring that the chosen surgical technique is the best fit for the individual patient’s biomechanical profile. This approach not only aims to restore knee stability but also to match the reconstructed knee’s function as closely as possible to its pre-injury state, thereby optimizing patient satisfaction and long-term joint health.
IV. Integrating Dyneelax into ACL Reconstruction Planning
The integration of the DYNEELAX® system into Anterior Cruciate Ligament (ACL) reconstruction planning signifies a paradigm shift towards a more data-driven, personalized approach to orthopedic surgery. By combining dynamic arthrometry measurements with Magnetic Resonance Imaging (MRI), surgeons can now tailor each surgical procedure to the unique biomechanical profile of the individual patient, thereby enhancing the precision and effectiveness of the intervention.
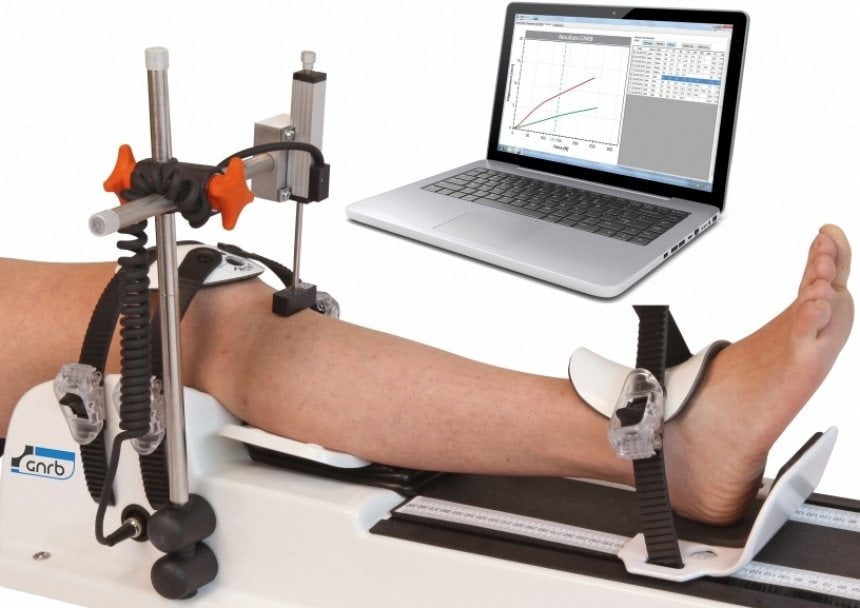
4.1 Comprehensive Preoperative Planning
The cornerstone of this advanced preoperative planning is the fusion of DYNEELAX®‘s dynamic assessments of knee stability with the anatomical insights provided by MRI. DYNEELAX®‘s ability to accurately measure Antero Posterior tibial Translation (APT) and Internal/External Tibial Rotation introduces a new dimension of knee function assessment, which, when combined with MRI, offers a holistic view of both the structural and functional aspects of the knee. This dual-analysis enables surgeons to identify specific patterns of instability and anatomical damage, thereby facilitating a more comprehensive and customized surgical plan that addresses all aspects of the knee’s biomechanical deficit.
4.2 Personalized Surgery Benefits
The benefits of such a personalized surgical approach are manifold. Precision surgery, informed by detailed preoperative data, significantly increases the likelihood of restoring the knee to its pre-injury state, optimizing postoperative stability, and reducing the risk of future injuries. Patients benefit from surgical interventions that are not only tailored to correct their specific biomechanical instabilities but also designed to match their individual anatomical configurations, thus ensuring that the reconstructed ACL behaves as naturally as possible.
Moreover, the strategic use of DYNEELAX® in surgical planning underscores its emerging role as an indispensable tool in ACL treatment. Its ability to provide a dynamic assessment of knee stability before surgery is instrumental in guiding the choice of surgical techniques, such as deciding between different tunnel placements or determining the necessity of additional procedures like Lateral Extra-Articular Tenodesis (LET) for enhanced rotational stability.
The integration of DYNEELAX® into ACL reconstruction planning is emblematic of the strides being made towards personalized medicine in orthopedics. It represents a significant advancement in ensuring that each patient receives the most appropriate, biomechanically sound, and effective treatment possible. As Dyneelax continues to be embraced by the orthopedic community, its role in enhancing surgical precision and patient outcomes in ACL reconstruction is set to become increasingly pivotal, marking a new era in the treatment of knee ligament injuries.
Conclusion
This exploration of ACL Reconstruction Techniques and the integration of the DYNEELAX® arthrometer system highlights the remarkable strides being made in personalized orthopedic surgery. The journey from traditional transtibial and transPortal approaches to more anatomically faithful methods such as outside-in, over-the-top, and all-inside techniques, underscores the orthopedic community’s commitment to improving surgical outcomes and patient recovery experiences. Each technique, with its unique advantages in addressing the biomechanical demands of the knee, showcases the complexity and innovation within the field of ACL reconstruction.
The introduction of DYNEELAX® into this sophisticated landscape has marked a significant leap forward. By enabling dynamic assessments of knee stability, Dyneelax has become a pivotal tool in the preoperative planning phase, offering surgeons a deeper insight into the specific instabilities and anatomical challenges presented by each case. Its role in guiding the selection of the most appropriate tunnel surgery technique, or in deciding the necessity of adjunctive procedures like the Lateral Extra-Articular Tenodesis (LET), cannot be overstated. The system’s capacity to tailor surgical strategies to the individual’s biomechanical profile embodies the essence of personalized medicine in orthopedics.
Future Perspectives in ACL reconstruction are bright, with ongoing advancements in diagnostic and surgical technologies promising even more personalized and effective treatment options. The integration of dynamic arthrometry, alongside evolving surgical techniques and a deeper understanding of knee biomechanics, is poised to further refine the art and science of ACL reconstruction. As Dyneelax and similar technologies become more integrated into clinical practice, the potential for achieving optimal patient outcomes through precision surgery becomes increasingly tangible.
In essence, the journey towards personalized ACL reconstruction, bolstered by technological innovations like Dyneelax, is an exciting and dynamic field of orthopedic surgery, promising improved stability, functionality, and satisfaction for patients navigating the road to recovery.
Medical References (Link in DOI)
- Silva, A., Sampaio, R., & Pinto, E. (2012). ACL reconstruction: comparison between transtibial and anteromedial portal techniques. Knee Surgery, Sports Traumatology, Arthroscopy, 20(5), 896-903. DOI: 10.1007/s00167-011-1645-3
- Sinha, S., Naik, A. K., Meena, D., Jain, V. K., & Arya, R. K. (2014). Creation of femoral tunnel by outside-in technique for ACL reconstruction: an analysis. Archives of Orthopaedic and Trauma Surgery, 134(12), 1709-1716. DOI: 10.1007/s00402-014-2078-5
- CarlLee, T., Ries, Z., Duchman, K., Gao, Y., Wolf, B., Amendola, A., Hettrich, C., & Bollier, M. (2017). Outside-In vs. Anteromedial Portal Drilling During Primary ACL Reconstruction: Comparison at Two Years. Iowa Orthopaedic Journal, 37, 117-122. PMCID: PMC5508260
- Nagai, K., Rothrauff, B. B., Li, R. T., & Fu, F. H. (2020). Over-the-top ACL reconstruction restores anterior and rotatory knee laxity in skeletally immature individuals and revision settings. Knee Surgery, Sports Traumatology, Arthroscopy, 28(2), 538-543. DOI: 10.1007/s00167-019-05719-5
- Mei, S., Li, R., Xiang, X., & Wang, W. (2022). [Research progress of anterior cruciate ligament reconstruction with over-the-top technique]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi, 36(9), 1166-1171. DOI: 10.7507/1002-1892.202203097
- Sarraj, M., de Sa, D., Shanmugaraj, A., Musahl, V., & Lesniak, B. P. (2019). Over-the-top ACL reconstruction yields comparable outcomes to traditional ACL reconstruction in primary and revision settings: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy, 27(2), 427-444. DOI: 10.1007/s00167-018-5084-2
- Min, B.-H., Song, H. K., Park, K. H., Kim, T. H., Park, D. Y., & Chung, J. Y. (2022). Biomechanical Evaluation of Modified ACL Reconstruction with Over-the-Top Augmentation Technique. Indian Journal of Orthopaedics, 56(5), 812-820. DOI: 10.1007/s43465-021-00597-x
- Nuelle, C. W., Balldin, B. C., Slone, H. S. (2022). All-Inside Anterior Cruciate Ligament Reconstruction. Arthroscopy, 38(8), 2368-2369. DOI: 10.1016/j.arthro.2022.06.001
- Bosco, F., Giustra, F., Ghirri, A., Cacciola, G., Massè, A., & Capella, M. (2023). All-Inside Anterior Cruciate Ligament Reconstruction Technique: Tips and Tricks. Journal of Clinical Medicine, 12(18), 5793. DOI: 10.3390/jcm12185793
- Connaughton, A. J., Geeslin, A. G., & Uggen, C. W. (2017). All-inside ACL reconstruction: How does it compare to standard ACL reconstruction techniques? Journal of Orthopaedics, 14(2), 241-246. DOI: 10.1016/j.jor.2017.03.002
- Schurz, M., Tiefenboeck, T. M., Winnisch, M., Syre, S., Plachel, F., Steiner, G., Hajdu, S., & Hofbauer, M. (2016). Clinical and Functional Outcome of All-Inside Anterior Cruciate Ligament Reconstruction at a Minimum of 2 Years’ Follow-up. Arthroscopy, 32(2), 332-337. DOI: 10.1016/j.arthro.2015.08.014
- Ro, K.-H., Kim, H.-J., & Lee, D.-H. (2018). The transportal technique shows better clinical results than the transtibial techniques for single-bundle anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 26(8), 2371-2380. DOI: 10.1007/s00167-017-4786-1
- Yau, W. P., Fok, A. W. M., & Yee, D. K. H. (2013). Tunnel positions in transportal versus transtibial anterior cruciate ligament reconstruction: a case-control magnetic resonance imaging study. Arthroscopy, 29(6), 1047-1052. DOI: 10.1016/j.arthro.2013.02.010
- Logan, J. S., Elliot, R. R., & Wilson, A. J. (2012). TransLateral ACL reconstruction: a technique for anatomic anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy, 20(7), 1289-1292. DOI: 10.1007/s00167-011-1745-0
- Cojean, T., Batailler, C., Robert, H., Cheze, L. (2023). Sensitivity repeatability and reproducibility study with a leg prototype of a recently developed knee arthrometer: The DYNEELAX®. Medicine in Novel Technology and Devices, 19, 100254. DOI: 10.1016/j.medntd.2023.100254