Anterior cruciate ligament (ACL) injuries are a significant concern for athletes across various sports, particularly in tennis, where rapid changes in direction and sudden stops put tremendous stress on the knees. As tennis continues to evolve into a faster and more physically demanding sport, the incidence of ACL injuries has become more prevalent, prompting a need for increased focus on effective prevention, diagnosis, and treatment strategies.
The ACL is crucial for maintaining knee stability and coordinating smooth joint movements. An injury to this ligament not only sidelines athletes for extended periods—often requiring surgical intervention and lengthy rehabilitation—but can also have lasting effects on their performance and, potentially, their long-term joint health. For tennis players, preserving knee function is essential, not just for competitive success but for future quality of life.
Recent advances in medical technology, such as robotic knee laxity arthrometers like the DYNEELAX® and GNRB®, have improved the accuracy of diagnosing ACL injuries. These tools measure knee joint laxity with high precision, aiding in the swift and accurate assessment necessary for effective treatment planning. However, while diagnostic advancements are crucial, they form just one part of the comprehensive approach needed to address ACL injuries in tennis.
This article delves into the various aspects of ACL injuries within the tennis world, from understanding the biomechanics of such injuries to exploring the latest in treatment protocols and preventive measures. By integrating insights from recent scientific studies, we aim to provide a well-rounded discussion that not only enhances understanding but also empowers players, coaches, and healthcare providers with knowledge to mitigate these injuries effectively. As the sport continues to grow in intensity and competitiveness, the insights from studies (L Y Griffin et al. – 2000), (Astrid Junge et al. – 2009), and (Fred Johansson et al. – 2022) among others, become ever more critical in shaping approaches to prevention and care, ensuring athletes can enjoy longer, healthier careers in tennis.
I. Background on ACL Injuries in Tennis

The anterior cruciate ligament (ACL) is one of the key ligaments that help stabilize the knee joint. Located centrally within the knee, it connects the femur (thigh bone) to the tibia (shin bone), playing a critical role in maintaining knee stability, especially during high-intensity activities involving pivoting, jumping, or sudden stops—movements that are all too common in tennis.
ACL injuries typically occur in sports settings due to either direct impact, which is less common in tennis, or, more frequently, through non-contact mechanisms such as abrupt deceleration, sharp directional changes, or awkward landings. These movements can overstretch the ACL beyond its tensile strength, leading to partial or complete tears. Research has shown that the dynamic nature of tennis, with its rapid accelerations and decelerations combined with rotational movements, places significant strain on the ACL, thus heightening injury risk (L Y Griffin et al. – 2000), (Fred Johansson et al. – 2022).
The impact of ACL injuries extends beyond the immediate physical damage. Athletes facing such injuries often undergo a long period of recovery that can last from six months to a year, involving both surgical intervention and extensive physiotherapy. Surgical approaches, primarily involving the reconstruction of the ligament with a graft, are common and necessary for athletes wishing to return to high levels of play. The recovery timeline not only affects the physical capabilities of players but also has psychological implications, as athletes often face challenges related to motivation, fear of re-injury, and the mental strain of prolonged rehabilitation (David J Biau et al. – 2007).
Moreover, the prevalence of ACL injuries varies by gender, with female athletes experiencing a higher incidence rate than their male counterparts in similar sports settings. This disparity is thought to be due to differences in biomechanics, hormonal influences, and neuromuscular conditioning, which can affect the way stress is distributed across the knee joint during athletic activities (Sally B Mountcastle et al. – 2007 ). Understanding these factors is crucial for developing targeted prevention and training programs that address the specific needs of all tennis players.
Prevention strategies are particularly important in this context. They often involve strength training, proprioceptive exercises, and technique adjustments, all aimed at reducing the load on the ACL during athletic movements. Specific programs designed to enhance knee stability and educate athletes about safe movement patterns can significantly decrease the likelihood of ACL injuries.
The emerging focus on preventive measures highlights the evolving understanding of ACL injuries within tennis and the broader athletic community. By integrating biomechanical research with clinical outcomes, the approach to managing ACL risks in tennis is becoming increasingly sophisticated, aiming not only to treat injuries but to prevent them, thus ensuring athletes can maintain long and healthy careers.
II. Diagnosis and Assessment of ACL Injuries
The accurate diagnosis and assessment of anterior cruciate ligament (ACL) injuries are crucial for determining the most effective treatment plan and for predicting recovery outcomes. The diagnostic process typically begins with a thorough physical examination and is followed by imaging techniques to confirm the extent of the injury.
2.1 Physical Examination
The clinical evaluation starts with a detailed physical examination, incorporating several specific tests designed to assess the structural integrity of the ACL. The Lachman test is one of the most sensitive tests for ACL tears, detecting abnormal forward movement of the tibia relative to the femur. The pivot shift test is another dynamic test that assesses the knee’s stability under rotational stress, simulating conditions that might cause the knee to “give out” during activity. The anterior drawer test also measures anterior tibial translation but in a seated position. These manual tests are crucial for initial assessments and are highly dependent on the examiner’s experience and technique. They help in establishing a preliminary diagnosis which directs further imaging studies.
2.2 Imaging Techiques
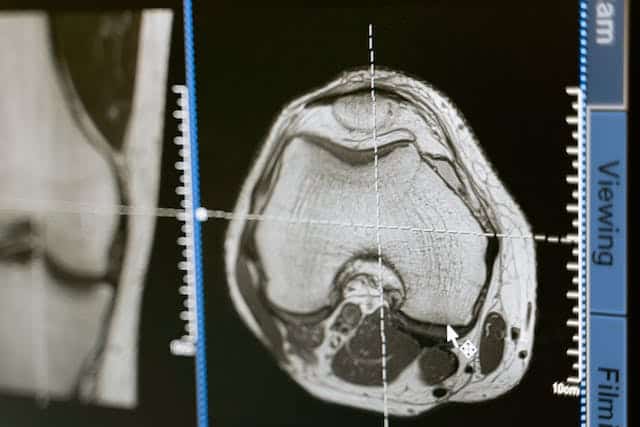
- MRI (Magnetic Resonance Imaging): MRI is the gold standard for visualizing the ACL and assessing its integrity post-injury. It not only confirms the presence of an ACL tear but also evaluates associated injuries such as damage to the menisci, cartilage, and other ligaments. MRI provides high-resolution images that allow for a detailed assessment of soft tissue structures, making it invaluable for surgical planning and assessing the feasibility of different treatment options.
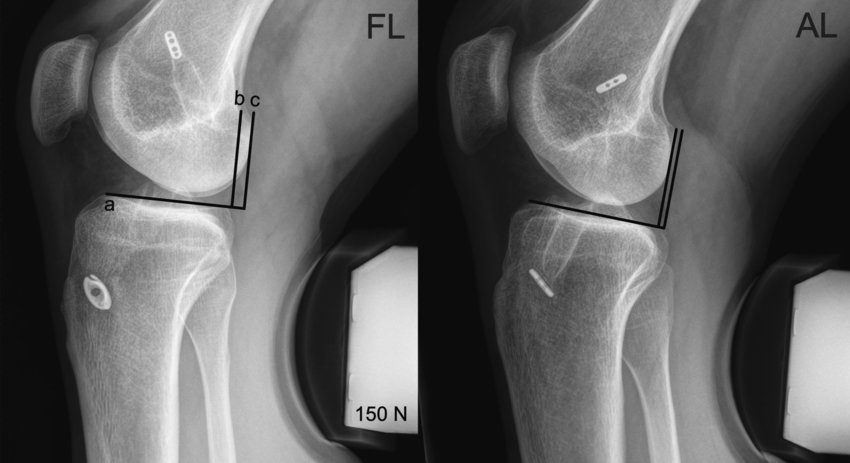
- X-rays: While X-rays are not used to visualize the ACL directly, they are crucial for evaluating the overall bone structure and alignment of the knee. X-rays help rule out associated bone injuries like fractures or a tibial spine avulsion, which can occur concurrently with ACL injuries. They are often the first imaging modality used to ensure there is no immediate bone injury complicating the ACL tear.
2.3 Ultrasound Imaging
- Ultrasound is an emerging tool in ACL injury diagnostics, appreciated for its ability to provide real-time imaging. This technology enables assessments of the knee, offering insights into the behavior of the ACL and surrounding tissues during movement. Although less common than MRI, ultrasound is advantageous for its non-invasiveness, absence of radiation exposure, and lower cost, making it suitable for repeated follow-ups.
2.4 Robotic Knee Laxity Arthrometers:
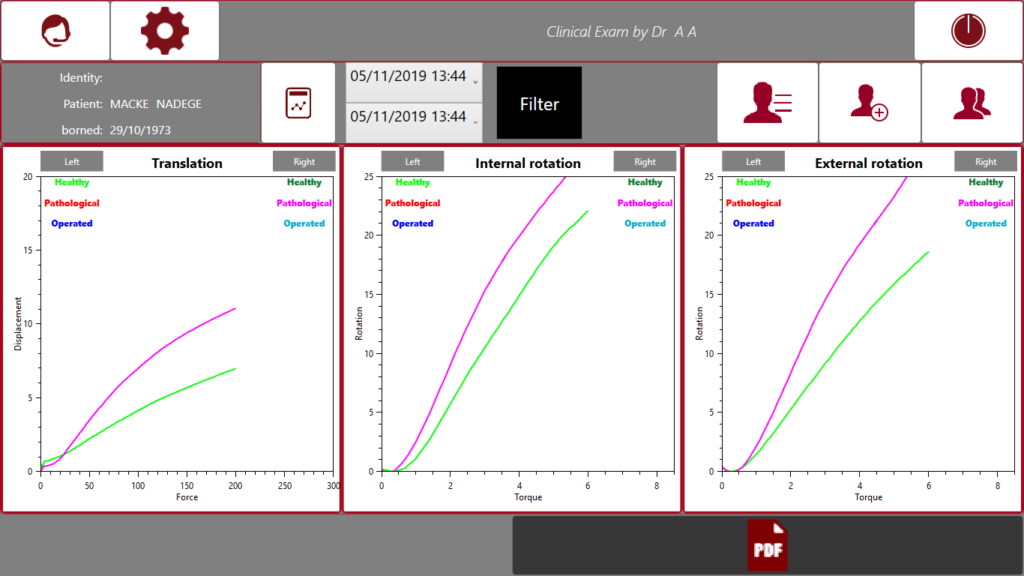
Robotic Knee Laxity Arthrometers: Tools like the DYNEELAX® and GNRB® arthrometers play a pivotal role in the modern diagnosis of ACL injuries by providing quantitative assessments of knee laxity.

- GNRB® Arthrometer: This device is highly valued for its precision and reliability in assessing knee laxity by means of applying anterior tibial translation only, as demonstrated in several studies. For example, the research by Magdic et al. (2023) highlighted its intra-rater reliability in measuring knee anterior laxity, showcasing its utility in clinical settings. Another study by Kayla Smith (2022) emphasized its reliability in measuring ACL stiffness and laxity, which is essential for accurate diagnosis and monitoring recovery.
- DYNEELAX® Arthrometer: A more recent advancement in knee diagnostics, the Dyneelax provides comprehensive measurements not only of translational but also rotational knee laxity. Nascimento et al. (2024) confirmed its reliability in providing these measurements under standardized conditions, underscoring its potential for enhancing ACL injury assessment and treatment protocols. Théo Cojean’s Dyneelax research (2023) focused on the Dyneelax’s sensitivity, repeatability, and reproducibility, further validating its application in clinical diagnostics for ACL injuries.
GNRB vs. MRI: Furthermore, another study from Théo Cojean (GNRB vs MRI) in 2023 has highlighted the effectiveness of the GNRB in diagnosing partial ACL ruptures, an area where MRI can sometimes be less definitive . The GNRB provides mechanical measurements of knee laxity that are not influenced by subjective interpretation, making it especially valuable for detecting subtle abnormalities in ligament integrity that might not be as apparent on MRI scans. It should be noted that DYNEELAX® has been developed after the GNRB and incorporates its technology.
These diagnostic tools, especially when combined with traditional examination and imaging, provide a robust framework for accurately diagnosing ACL injuries. They offer objective data that enhance our understanding of the injury’s nature and severity, which is essential for tailoring individualized treatment plans. The integration of devices like DYNEELAX® and GNRB® into the diagnostic process marks a significant advancement in sports medicine, offering a level of precision and reproducibility that manual examinations cannot achieve. This approach ensures that treatment strategies are based on detailed and accurate diagnostic information, leading to better recovery outcomes for patients with ACL injuries.
III. Treatment and Rehabilitation of ACL Injuries
The treatment and rehabilitation of anterior cruciate ligament (ACL) injuries in tennis players involve a multifaceted approach that includes surgical intervention and a carefully structured rehabilitation process. This treatment strategy aims to restore knee stability, function, and prevent long-term complications such as osteoarthritis.
3.1 Surgical Treatment
Surgical reconstruction of the ACL is generally recommended for athletes, particularly those involved in sports requiring pivot movements like tennis. The surgery typically involves replacing the torn ligament with a graft, which can be sourced from the patellar tendon, hamstring tendon, or a donor tissue. This graft helps to stabilize the knee and allows the athlete to eventually return to sports.
3.2 Post-Surgical Rehabilitation
Rehabilitation following ACL reconstruction is crucial and is typically phased over several months:
Initial Recovery: Focus on reducing inflammation, regaining range of motion, and gentle strengthening exercises.
Intermediate Phase: Incorporates more vigorous strength training and begins to reintroduce sports-specific skills.
Advanced Rehabilitation: Focuses on restoring full strength, agility, and function, with gradual return to sport-specific drills.
Throughout these phases, the application of advanced diagnostic and assessment tools such as the DYNEELAX® and GNRB® arthrometers are crucial. These devices provide precise measurements of knee laxity and help tailor rehabilitation to individual needs. Click here to read our rehabilitation programs following ACL Reconstruction surgery.
3.3 Integration of Recent Studies
Recent studies have shed light on the dynamics of graft behavior and the effectiveness of rehabilitation protocols:
- Forelli et al., 2023: Highlights the importance of personalized rehabilitation protocols post-ACL surgery. The study emphasizes early mobilization and controlled physical therapy to optimize outcomes and prevent stiffness.
- Semay et al., 2016: This study analyzed the evolution of anteroposterior laxity over time, using the GNRB device. It found significant improvements in knee stability at 12 months post-operation, suggesting the efficacy of gradual load increase during rehabilitation.
- Pouderoux et al., 2019: Examined joint laxity and graft compliance using GNRB, noting that changes in graft properties are most pronounced in the first year post-surgery. This underscores the need for careful monitoring during this period to adjust rehabilitation efforts accordingly.
- Nouveau, Robert, Viel, 2017: Discussed the impact of early rehabilitation on graft stiffness and compliance, indicating that early and appropriate mechanical solicitations are critical in maintaining graft integrity and function.
These insights emphasize the importance of a nuanced approach to ACL rehabilitation, integrating continuous monitoring with physical therapy to adjust the recovery process based on real-time feedback from diagnostic tools like GNRB and Dyneelax. Such an approach not only aids in a safer return to sport but also enhances long-term knee health and athletic performance.
IV. Prevention Strategies for ACL Injuries in Tennis
Effective prevention strategies for ACL injuries in tennis players are crucial to reduce the incidence and severity of these injuries. These strategies involve a combination of strength training, proper technique, and education to address the specific risks associated with tennis.

4.1 Strength and Conditioning Programs
Emphasizing neuromuscular training programs can significantly decrease the risk of ACL injuries. These programs focus on improving strength, balance, agility, and proprioceptive abilities. Research has shown that plyometric exercises combined with strength training reduce ACL injury rates by enhancing muscular reactions and improving joint stability. Exercises that strengthen the hamstring and quadriceps can also help stabilize the knee and balance the forces exerted on the ACL during dynamic movements in tennis (L Y Griffin et al. – 2000).
4.2 Technique Modification
Proper technique is essential in tennis to avoid undue stress on the knees. Coaches and trainers should emphasize techniques that reduce risky movements, such as avoiding hyperextension or excessive pivoting on the knee. Training should also include teaching athletes the correct way to land from jumps and how to effectively change direction, which can mitigate the risk of ACL injuries (Astrid Junge et al. – 2009)
4.3 Use of Supportive Equipment
Wearing appropriate footwear that offers good grip and stability can prevent the foot from sliding or sticking during play, reducing torsional knee stresses. Some studies suggest that knee braces might provide additional support, although their efficacy in preventing ACL injuries specifically in tennis players is still debated and may depend on the player’s history of previous injuries.
4.4 Educational Interventions
Educating players about the risk factors and early signs of ACL injuries can lead to earlier detection and management, potentially reducing the severity of injuries. Awareness programs for coaches, athletes, and parents about the importance of prevention programs, proper warm-up routines, and recognizing fatigue, which can impair neuromuscular control, are also vital components of injury prevention.
Implementing these preventive measures requires a collaborative effort from coaches, trainers, physiotherapists, and the athletes themselves. By incorporating structured warm-up programs, focused strength and agility training, and continuous education on injury prevention, tennis players can significantly reduce their risk of sustaining an ACL injury and thereby enhance their playing longevity and performance.
V. Future Directions in ACL Injury Management and Prevention in Tennis

The management and prevention of ACL injuries in tennis are poised for significant advancements with the integration of technology and personalized medicine. Future strategies are likely to focus on early detection, innovative treatment methods, and personalized intervention plans.
Biomechanical Monitoring: Advancements in wearable technology will enable continuous monitoring of athletes’ biomechanics in real-time. Devices can potentially alert players and coaches to dangerous movement patterns or excessive strain on the ACL during play. This could allow for immediate corrections in technique or intensity, potentially preventing injuries before they occur.
Genetic Profiling: Research into the genetic factors influencing susceptibility to ACL injuries could lead to breakthroughs in personalized injury prevention. Identifying individuals at higher genetic risk for ligament injuries could prompt early preventive interventions, tailored strength and conditioning programs, or even guide decisions about participation in certain sports activities.
Tissue Engineering and Regenerative Medicine: The future of ACL reconstruction may also see innovations through tissue engineering and regenerative medicine. Research is ongoing into scaffold technologies that promote ligament healing and regeneration. These techniques aim to enhance the biological healing process, potentially leading to faster recovery times and reduced rates of re-injury.
Robotics and AI in Rehabilitation: The use of robotic systems like DYNEELAX® and GNRB® and artificial intelligence in rehabilitation will likely become more prevalent. These systems can provide highly precise and personalized rehabilitation protocols based on the specific needs and recovery progress of the athlete. For instance, robotics can assist in ensuring that exercises are performed with correct form and appropriate resistance, enhancing the effectiveness of rehabilitation.
Holistic Approach to Athlete Health: Finally, there is a growing recognition of the need for a holistic approach to athlete health, which considers not only physical conditioning but also nutritional, psychological, and lifestyle factors that contribute to the risk of ACL injuries. Integrating these aspects into training and prevention programs could help athletes not only recover from injuries but also optimize their overall health and performance.
By embracing these future directions, the field of sports medicine, particularly concerning ACL injuries in tennis, will likely provide enhanced outcomes for prevention, treatment, and recovery, ultimately benefiting athletes’ careers and well-being.
Conclusion
This article has explored the multifaceted aspects of ACL injuries in tennis, providing insights into their mechanisms, diagnosis, treatment, and effective strategies for prevention. We have emphasized the critical role of early detection and accurate diagnosis using advanced tools like the DYNEELAX® and GNRB® arthrometers, which enhance the precision in assessing knee laxity. Surgical interventions coupled with comprehensive rehabilitation programs are pivotal in restoring knee functionality and aiding athletes in their return to sport.
Furthermore, we discussed preventive measures that encompass strength training, technique refinement, and educational initiatives aimed at reducing the incidence of ACL injuries. These interventions are vital for both novice and professional players in mitigating injury risks during high-demand sports activities.
Looking forward, the integration of wearable technology, genetic profiling, and advancements in tissue engineering represents promising areas for enhancing ACL injury management. These innovations hold the potential to personalize treatment plans and optimize recovery processes, tailored to individual athletes’ physiological and biomechanical profiles.
In light of these discussions, there is a clear call to action for continued education, research, and investment in preventive measures and rehabilitation technologies. Stakeholders in sports medicine and athletic training should prioritize these advancements to not only improve outcomes for athletes with ACL injuries but also to prevent these injuries before they occur. By fostering a deeper understanding and implementing these cutting-edge strategies, we can better support tennis players in achieving longer, healthier, and more successful careers.
Medical References
- Griffin, L. Y., Agel, J., Albohm, M. J., Arendt, E. A., Dick, R. W., Garrett, W. E., … & Wojtys, E. M. (2000). Noncontact anterior cruciate ligament injuries: Risk factors and prevention strategies. Journal of the American Academy of Orthopaedic Surgeons, 8(3), 141-150. DOI: 10.5435/00124635-200005000-00001.
- Junge, A., Engebretsen, L., Mountjoy, M. L., Alonso, J. M., Renström, P. A. F. H., Aubry, M. J., & Dvorak, J. (2009). Sports injuries during the Summer Olympic Games 2008. American Journal of Sports Medicine, 37(11), 2165-2172. DOI: 10.1177/0363546509339357.
- Johansson, F., Tranaeus, U., Asker, M., Skillgate, E., & Johansson, F. (2022). Athletic Identity and Shoulder Overuse Injury in Competitive Adolescent Tennis Players: The Smash Cohort Study. Frontiers in Sports and Active Living, 4, Article 940934. DOI: 10.3389/fspor.2022.940934.
- Biau, D. J., Tournoux, C., Katsahian, S., Schranz, P., & Nizard, R. (2007). ACL reconstruction: A meta-analysis of functional scores. Clinical Orthopaedics and Related Research, 458, 180-187. DOI: 10.1097/BLO.0b013e31803dcd6b.
- Navon, L., Chen, L. H., Cowhig, M., & Wolkin, A. F. (2023). Two decades of nonfatal injury data: A scoping review of the National Electronic Injury Surveillance System-All Injury Program, 2001-2021. Injury Epidemiology, 10(1), 44. DOI: 10.1186/s40621-023-00455-4.
- Magdić M, Gošnak Dahmane R, Vauhnik R. (2023). Intra-rater reliability of the knee arthrometer GNRB® for measuring knee anterior laxity in healthy active subjects. Journal of Orthopaedics. DOI: 10.1016/j.jor.2023.03.016
- Smith K, Miller N, Laslovich S. (2022). The Reliability of the GNRB® Knee Arthrometer in Measuring ACL Stiffness and Laxity: Implications for Clinical Use and Clinical Trial Design. Int J Sports Phys Ther, 17(6), 1016-1025. DOI: 10.26603/001c.38252
- Nascimento, N., Kotsifaki, R., Papakostas, E., Zikria, B. A., Alkhelaif, K., Hagert, E., Olory, B., D’Hooghe, P., & Whiteley, R. (2024). DYNEELAX Robotic Arthrometer Reliability and Feasibility on Healthy and Anterior Cruciate Ligament Injured/Reconstructed Persons. Translational Sports Medicine, 2024(1), 1-5. DOI: 10.1155/2024/3413466
- Cojean, T., Batailler, C., Robert, H., Cheze, L. (2023). Sensitivity repeatability and reproducibility study with a leg prototype of a recently developed knee arthrometer: The DYNEELAX®. Medicine in Novel Technology and Devices, 19, 100254. DOI: 10.1016/j.medntd.2023.100254
- Cojean T, Batailler C, Robert H, Cheze L. (2023). GNRB® laximeter with magnetic resonance imaging in clinical practice for complete and partial anterior cruciate ligament tears detection: A prospective diagnostic study with arthroscopic validation on 214 patients. Knee, 42, 373-381. DOI: 10.1016/j.knee.2023.03.017
- Forelli F, Le Coroller N, Gaspar M, et al. (2023). Ecological and Specific Evidence-Based Safe Return To Play After Anterior Cruciate Ligament Reconstruction In Soccer Players: A New International Paradigm. IJSPT. Published online April 2, 2023. DOI: 10.26603/001c.73031
- Semay, B., Rambaud, A., Philippot, R., Edouard, P. (2016). Evolution of the anteroposterior laxity by GnRB at 6 9 and 12 months post-surgical anterior cruciate ligament reconstruction. DOI: 10.1016/j.rehab.2016.07.045
- Pouderoux, T., Muller, B., Robert, H. (2019). Joint laxity and graft compliance increase during the first year following ACL reconstruction with short hamstring tendon grafts.. DOI: 10.1007/s00167-019-05711-z
- Nouveau, S., Robert, H., Viel, T. (2017). ACL Grafts Compliance During Time: Influence of Early Solicitations on the Final Stiffness of the Graft after Surgery. Journal of Orthopedic Research and Physiotherapy, 3(1), 035. DOI: 10.24966/ORP-2052/100035