Anterior Cruciate Ligament (ACL) injuries represent a significant and impactful pathology within the realm of sports medicine, particularly in basketball—a sport characterized by its high intensity and dynamic movements. The prevalence of ACL injuries in basketball is not just a matter of concern due to the frequency at which they occur but also because of the profound implications they have on an athlete’s career, encompassing aspects such as return-to-play timelines, performance post-recovery, and the overarching risk of future osteoarthritis. This concern is amplified in female athletes, who are shown to have a higher incidence rate of ACL injuries compared to their male counterparts, a disparity that underscores the need for targeted preventive strategies and interventions (Read Ryu et al – 2018)(1).
The management of ACL injuries encompasses a multifaceted approach, involving accurate diagnosis, effective rehabilitation, and the implementation of preventative measures. In this context, the advent of knee robotic arthrometers, such as Dynelax and GNRB, has heralded a new era in the diagnostic landscape. These sophisticated devices offer unparalleled precision in assessing ligament laxity, thereby playing a pivotal role in the early detection of injuries and the monitoring of rehabilitation progress. Although their application is a cornerstone in the technological advancement of ACL injury management, the primary focus of our discourse remains on the injury itself—its mechanisms, prevention, and the impact on athletic performance.
As we delve into the intricacies of ACL injuries in basketball, it is imperative to recognize the significance of a comprehensive approach that integrates the latest in diagnostic technology with evidence-based clinical practices. This harmonious blend of innovation and expertise is crucial in not only mitigating the impact of ACL injuries on athletes but also in paving the way for their successful return to the sport they are passionate about. The subsequent sections will explore the current state of knowledge regarding ACL injuries in basketball, drawing on recent scientific studies to shed light on this pressing issue.
I. Understanding ACL Injuries in Basketball

Understanding the complexity and implications of Anterior Cruciate Ligament (ACL) injuries in basketball is paramount for clinicians, athletes, and coaches alike. The dynamics of basketball, characterized by rapid direction changes, jumping, and physical contact, present a unique set of challenges and risks for ACL integrity. This section delves into the epidemiology, biomechanics, and situational patterns associated with these injuries, informed by recent scientific investigations.
Epidemiology and Gender Disparities: Studies have consistently demonstrated a higher incidence of ACL injuries among female athletes compared to males within the realm of basketball. This gender disparity in ACL injury rates is attributed to a combination of anatomical, hormonal, biomechanical, and neuromuscular factors. Females exhibit differences in knee alignment, ligament laxity, muscle strength, and landing mechanics, which may increase their susceptibility to ACL injuries during high-intensity basketball activities (Read Stojanović et al. – 2023)(2).
Biomechanical Insights and Injury Mechanisms: Advanced research, including comprehensive video analyses of ACL injuries in National Basketball Association (NBA) players, has shed light on the biomechanics and situational patterns associated with these incidents. Such studies have meticulously evaluated the joint kinematics and game situations at the time of injury, revealing that a significant proportion of ACL injuries occur without direct contact. The analysis of player movements and court situations has highlighted the pivotal moments when athletes are most vulnerable, such as during landing from a jump or executing rapid direction changes (Read Gill et al. 2023 (3) and Krosshaug et al. 2007(4)).
Situational Analysis of Injuries: The context within which ACL injuries occur in basketball has been extensively studied, offering valuable insights into the most hazardous actions and phases of play. For instance, non-contact injuries often result from improper landing techniques or sudden deceleration combined with directional change. This understanding underscores the importance of situational awareness and reinforces the need for targeted preventive training programs designed to modify risky behaviors and improve neuromuscular control (Read Krosshaug et al. 2007 (4)).
Moreover, the distinction between contact and non-contact injuries in basketball further emphasizes the multifactorial nature of ACL injuries. While direct impact can certainly lead to ACL ruptures, the majority of injuries in basketball arise from intrinsic factors related to the athlete’s movement patterns. Addressing these intrinsic risk factors through individualized training and intervention programs can significantly reduce the incidence of ACL injuries (Read Gill et al. 2023 (3)).
The comprehensive understanding of ACL injuries in basketball requires an interdisciplinary approach, integrating insights from epidemiology, biomechanics, and clinical practice. Recognition of the gender-specific risk factors, coupled with a detailed analysis of the mechanisms and situational contexts of these injuries, provides a solid foundation for developing effective prevention and rehabilitation strategies. The ultimate goal is to mitigate the risk of ACL injuries in basketball players, thereby enhancing their safety, performance, and longevity in the sport. The evolving landscape of ACL injury research continues to offer promising avenues for advancements in prevention, diagnosis, and treatment, promising a brighter future for athletes affected by these challenging injuries.



II. Advances in Prevention and Performance Post-Injury
Advancements in the prevention and management of Anterior Cruciate Ligament (ACL) injuries within the basketball community have been noteworthy, marked by an increasing emphasis on evidence-based interventions and a deeper understanding of post-injury performance outcomes. The integration of scientific research into practical applications has led to the development of targeted injury prevention programs and refined rehabilitation protocols, aiming to not only reduce the incidence of ACL injuries but also optimize recovery and performance post-reconstruction.
2.1 Prevention Through Neuromuscular Training
A significant breakthrough in ACL injury prevention has been the implementation of neuromuscular training programs. These programs are designed to enhance proprioceptive abilities, improve landing mechanics, and increase muscular strength and coordination. For instance, a hip-focused injury prevention program demonstrated a substantial reduction in the incidence of ACL injuries among female collegiate basketball players. The study highlighted an impressive decrease in noncontact ACL injury rates, attributing success to the rigorous compliance with the preventative training protocols (Read Omi et al. 2018). This underscores the critical role of preventive neuromuscular training in mitigating ACL injury risks, especially in high-risk populations.
2.2 Recovery and Return to Play
The journey from ACL reconstruction (ACLR) to return to play (RTP) is complex and multifaceted, demanding a strategic approach that addresses both physical and psychological aspects of recovery. Research focusing on NBA players post-ACLR has revealed that while the rate of RTP is high, the path to regaining pre-injury performance levels may extend beyond a single season. Younger athletes and those with less professional experience tend to exhibit higher RTP rates, suggesting that age and playing experience are significant factors influencing recovery outcomes (Read DeFroda et al. 2021 (6)).
Moreover, studies examining the Women’s National Basketball Association (WNBA) players post-ACLR have highlighted similar trends regarding workload and performance metrics. Initial decreases in games played and minutes per game were observed; however, a gradual recovery to baseline workload levels was typically achieved within three years post-injury (Read Tramer et al. 2020 (7)). These insights are crucial for setting realistic expectations and tailoring rehabilitation programs to individual athlete needs, ultimately facilitating a successful and sustainable RTP.
2.3 Role of Diagnostic Tools in Injury Management
In the backdrop of these advancements, the utilization of knee robotic arthrometers like DYNEELAX® and GNRB® has gained prominence. These devices offer precise measurements of ligament laxity, enriching the diagnostic process and enabling personalized rehabilitation strategies. By accurately assessing the extent of injury and recovery progress, clinicians can make informed decisions regarding the timing of RTP and necessary adjustments in rehabilitation protocols.
The integration of scientific evidence into clinical practice has significantly advanced the prevention and management of ACL injuries in basketball. Through dedicated injury prevention programs and tailored rehabilitation strategies, there is a tangible impact on reducing injury rates and enhancing athlete recovery. Continuous research and technological innovation, such as the application of knee robotic arthrometers, further solidify the foundation for evidence-based approaches, ensuring athletes receive the highest standard of care. As the field evolves, the collaboration between researchers, clinicians, and athletes will remain pivotal in overcoming the challenges associated with ACL injuries, paving the way for safer sports participation and optimal performance outcomes.
III. Role of Knee Robotic Arthrometers in ACL Injury Management
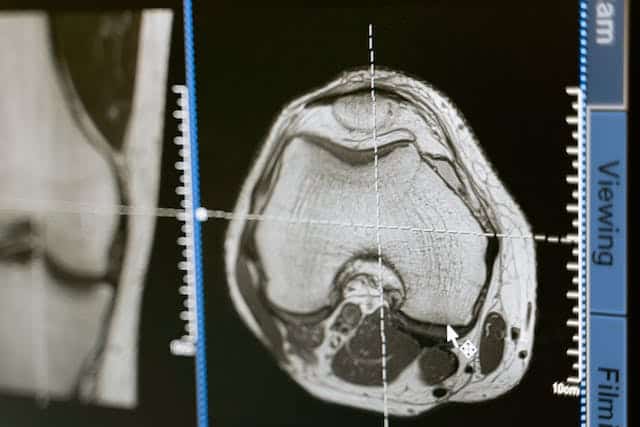
The management and diagnosis of Anterior Cruciate Ligament (ACL) injuries have significantly progressed with the advent of knee robotic arthrometers like the DYNEELAX® and GNRB®. These state-of-the-art diagnostic tools offer a dynamic examination of knee stability, presenting an innovative complement to the traditional magnetic resonance imaging (MRI) scans traditionally used in ACL injury evaluations.
3.1 Enhanced Diagnosis with Knee Robotic Arthrometers
Knee robotic arthrometers have revolutionized the diagnosis of ACL injuries by providing a dynamic assessment of knee stability. Unlike MRI, which offers a static analysis of knee structures, these arthrometers measure the mechanical response of the knee to specific forces, thereby identifying subtle instabilities not always apparent on MRI scans. This is particularly beneficial for the diagnosis of partial ACL ruptures (Read Cojean – 2023 (8)), where robotic arthrometers have shown their superiority.
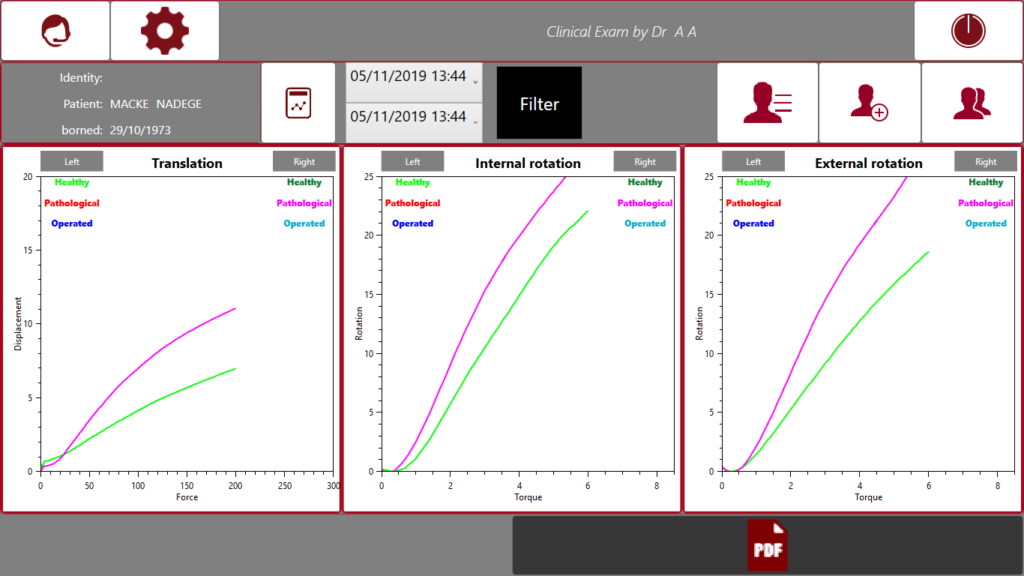
The GNRB® arthrometer focuses on measuring anterior tibial translation. In contrast, the DYNEELAX® system offers a more comprehensive evaluation, assessing both translation and rotation to give a complete picture of knee stability. This distinction underscores the importance of selecting the appropriate diagnostic tool based on the specific clinical scenario and the information needed to guide treatment planning.

The advancements in the diagnosis of ACL injuries through knee robotic arthrometers, particularly the DYNEELAX® and GNRB® systems, have been substantiated by several pivotal studies. These studies offer compelling evidence on the utility of these devices in enhancing the accuracy of ACL injury assessments.
The GNRB® arthrometer has been showcased for its reliable measures of knee anterior laxity, which is crucial for assessing the integrity of the anterior cruciate ligament. A study conducted by Magdic et al. in 2023 (9) highlighted the device’s intra-rater reliability for measuring knee anterior laxity in healthy active subjects. The study demonstrated good intra-rater reliability for the GNRB® measurements at forces of 134 N and 200 N.
Further emphasizing the importance of reliable diagnostic tools, 2023 Smith et al. (10) explored the reliability of the GNRB® Knee Arthrometer in measuring ACL stiffness and laxity. Their research underscored the clinical value of reliable and valid measures of ACL stiffness and laxity, providing crucial insights for clinical use and the design of clinical trials.
A groundbreaking study introduced the Dyneelax arthrometer, focusing on its sensitivity, repeatability, and reproducibility. This 2023 study by Cojean et al. (11) positioned the Dyneelax as a versatile diagnostic tool capable of assessing various aspects of knee stability, including both translation and rotation. Such comprehensive assessments are instrumental in forming a holistic understanding of knee mechanics following ACL injuries.
Together, these studies validate the efficiency of both GNRB® and Dyneelax in diagnosing ACL injuries. They highlight a significant shift towards more dynamic and comprehensive assessments, moving beyond the limitations of static imaging techniques like MRI.
3.2 Complementary Use with MRI
It’s crucial to underscore that the objective is not to replace MRI but to use these arthrometers in conjunction with it. MRI remains invaluable for its detailed visualization of soft tissue structures, allowing clinicians to identify concomitant injuries such as meniscal tears or cartilage damage that may accompany ACL ruptures. The combination of MRI’s detailed soft tissue visualization and the dynamic evaluation provided by knee robotic arthrometers equips clinicians with a comprehensive dataset, ensuring optimal treatment and rehabilitation strategies are employed. This collaborative approach underscores the importance of integrating both static and dynamic diagnostic tools for a full spectrum evaluation of ACL injuries, paving the way for personalized rehabilitation programs informed by precise, objective data.
3.3 Personalized Rehabilitation Programs
The precise measurements obtained from knee robotic arthrometers are instrumental in designing personalized rehabilitation programs. By quantifying the degree of instability and identifying specific mechanical deficits, clinicians can develop targeted exercise regimes that address the individual’s unique challenges. This customization is crucial for optimizing recovery outcomes, enhancing the efficacy of rehabilitation efforts, and minimizing the risk of re-injury.
Furthermore, the ability to monitor progress objectively through repeated measurements allows for real-time adjustments to the rehabilitation program. This dynamic approach ensures that the rehabilitation process remains aligned with the patient’s recovery trajectory, facilitating a more efficient and effective return to function. Integrating knee robotic arthrometers in the rehabilitation process following ACL reconstruction is supported by several studies, each highlighting the device’s utility in personalizing rehabilitation programs.
Semay et al. (2016) (12) explored the evolution of tibiofemoral anterior laxity during the return to sport post-ACL reconstruction, employing the GNRB® arthrometer for dynamic measurements. The study observed significant changes in anterior-posterior laxity between 9 and 12 months postoperatively, underscoring the significance of dynamic laxity assessment in guiding return-to-sport decisions. The findings suggest that rehabilitation programs should be cautiously progressed, especially in the critical period before ligament laxity stabilizes.
Pouderoux et al. (2019) (13) focused on joint laxity and graft compliance within the first year after ACL reconstruction using short hamstring tendon grafts, measured using the GNRB® arthrometer. The study highlighted a phase of relative weakness between the first and ninth postoperative month, indicating the importance of monitoring joint laxity and graft compliance for optimizing the rehabilitation timeline and preventing premature return to sports.
Nouveau et al. (2017) (14) investigated the impact of early solicitations on the final stiffness of ACL grafts post-surgery. Through precise measurements obtained from the GNRB® arthrometer, the study revealed how early, controlled biomechanical constraints are crucial for maintaining optimal graft compliance. This underscores the necessity for personalized, carefully monitored rehabilitation protocols that consider the evolving biomechanical properties of the ACL graft.
Forelli et al. (2023) (15) emphasized an ecological and evidence-based approach to return to play (RTP) after ACL reconstruction. Although not directly mentioning arthrometers, the study aligns with the principle of using objective measures to inform rehabilitation and RTP decisions. This approach advocates for the inclusion of functional and situational tests, highlighting the importance of tailoring rehabilitation to the individual’s specific recovery trajectory and sports demands.
Collectively, these studies advocate for the incorporation of knee robotic arthrometers in ACL rehabilitation, offering a foundation for more effective and personalized rehabilitation programs that are closely aligned with each patient’s specific needs and recovery progress.
IV. Strategies for ACL Injury Prevention

Strategies for Anterior Cruciate Ligament (ACL) injury prevention have evolved significantly, incorporating evidence-based practices aimed at reducing the high incidence of these debilitating injuries, especially in sports like basketball that demand high levels of agility and knee stability. Central to these strategies is the recognition of stiff landings as a pivotal risk factor for ACL injuries. Research has shown that athletes, particularly females, who exhibit biomechanically inefficient landing techniques are at an increased risk of ACL injuries (Read Leppänen et al – 2017).
The importance of incorporating biomechanical adjustments into training programs to mitigate this risk cannot be overstated. Training aimed at enhancing neuromuscular control, promoting soft landings, and increasing lower limb strength is crucial. Studies have underscored the efficacy of neuromuscular training programs in significantly reducing ACL injury rates by improving landing mechanics and knee stability among athletes.
Furthermore, the process of returning to sport (RTS) after ACL reconstruction demands a carefully structured approach, with a particular emphasis on task-based rehabilitation (Read Waters -2012). This approach is especially pertinent for basketball players, whose sport-specific demands include rapid changes in direction, jumping, and landing. Rehabilitation programs should, therefore, be tailored to simulate basketball-specific tasks, progressively preparing the athlete for the demands of the sport. The utilization of dynamic knee testing with tools like the DYNEELAX® and GNRB® arthrometer has been shown to offer valuable insights into the knee’s biomechanical status, facilitating a more informed and personalized RTS decision-making process. This aligns with recommendations for a cautious, criteria-based progression through the rehabilitation stages, ensuring that the athlete achieves optimal biomechanical function before RTS.
Recent studies, such as those by Semay et al. (2016), Nouveau et al. (2017), Pouderoux et al. (2019) and Forelli et al. (2023) have contributed significantly to our understanding of the biomechanical changes and recovery trajectories following ACL reconstruction. These insights underscore the necessity of a multifaceted approach to ACL injury prevention and rehabilitation, which incorporates biomechanical assessments, targeted training interventions, and a sport–specific focus in rehabilitation to effectively reduce injury rates and support a safe and successful return to play.
Moreover, Taylor et al. (2018) emphasized that while ACL injury prevention programs have shown success in sports like soccer (Click here to read our full article on ACL injuries in Soccer), their effectiveness in women’s basketball could be enhanced by focusing on sport-specific biomechanical adaptations. This study underscores the need for targeted injury prevention programs that account for the unique demands of basketball, such as jump-landing activities, to mitigate ACL injury risks .
Weir et al. (2021) contributed to the framework for preventing ACL injuries by focusing on biomechanically informed approaches. These approaches include modifying athletes’ techniques to reduce knee loads, enhancing muscle support around the knee, and improving perception during dynamic sports tasks. This comprehensive view reinforces the necessity of a multifaceted approach to ACL injury prevention, integrating technique modification, strength training, and cognitive strategies .
A 12-year prospective study by Omi et al. (2018) demonstrated the effectiveness of a hip-focused ACL injury prevention program in female collegiate basketball players. This long-term intervention significantly reduced ACL injury incidence, highlighting the importance of hip joint function training in ACL injury prevention programs for basketball players.
Finally, a systematic review and meta-analysis conducted by Sugimoto et al. (2016) provided evidence-based best-practice guidelines for preventing ACL injuries. The study recommended targeting younger athletes with NMT programs led by trained implementers, emphasizing lower body strength exercises and landing stabilization to reduce ACL injury risk. This research underscores the critical role of structured, comprehensive NMT programs in ACL injury prevention
V. Case Studies - Additional Arthrometer Scientific Reviews
5.1 Pre-Operative Clinical Validation
The section begins by underscoring the importance of precise and reliable pre-operative assessments in ACL reconstruction surgeries. It emphasizes the role of advanced diagnostic tools, particularly the DYNEELAX® and GNRB® arthrometers, in enhancing the accuracy of knee injury evaluations. These technologies represent significant improvements over traditional methods, offering clinicians a comprehensive and objective analysis critical for optimal surgical planning and outcomes.
5.1.1 Automated Anterior/Posterior Tibial Translation Analysis:
The GNRB®/DYNEELAX® robotic arthrometer, an advancement over manual methods like the Lachman test, offers precise, consistent measurements for ACL and PCL diagnostics. It overcomes the subjectivity of manual tests by applying uniform force and measuring tibial translation.
Studies validating the GNRB®:
- 2023, Théo Cojean et al.(8): Demonstrated GNRB®’s higher sensitivity (73.77%) compared to MRI (29.51%) in detecting partial ACL tears.
- 2022, Miha Magdič et al.(9): Confirmed good intra-rater reliability of the GNRB® in measuring knee anterior laxity.
- 2015, Klouche et al.(22): Proved GNRB®’s diagnostic accuracy in identifying complete ACL tears.
- 2017, Jenny et al.(23): Validated GNRB® for measuring anterior tibial translation.
- 2022, Kayla Smith et al.(10): Highlighted GNRB®’s reliability in assessing ACL stiffness and laxity.
- And Many more…
5.1.2 Medial/Lateral Tibial Rotation Assessments:
The DYNEELAX® arthrometer is a significant development for measuring translation & rotational stability, surpassing the pivot shift test’s subjective limitations.
It provides precise assessments of medial and lateral knee rotation and extends to analyze the ACL, the PCL, the Anteromedial (AM), Posterolateral (PL), Anterolateral (AL), and Posteromedial (PM) corners of the knee. It should be noted that all the studies of the GNRB can also be applied to the DYNEELAX® because GNRB® technology has been incorporated in the DYNEELAX®.
Studies supporting DYNEELAX®‘s Rotation Analysis (We focus on rotation assessments here as translation has just been put forward with the GNRB®):
- 2014, Mouton et al.(24): Emphasized the importance of combining anterior and rotational laxity measurements.
- 2015, Mouton et al.(25): Validated the combined measurement approach.
- 2016, Nicolas Ruiz et al.(26): Explored the ACL’s and anterolateral structures’ roles in knee rotational dynamics.
- 2017, Senioris et al.(27): Confirmed the importance of assessing rotational laxity with anterior translation.
- 2023, Théo Cojean et al.(11): Evaluated the sensitivity, repeatability, and reproducibility of the Dyneelax.
- And Many more…
5.2 Post-Operative Clinical Validation
Postoperative rehabilitation following ACL surgery is enhanced by the use of arthrometer measurements, particularly with devices like the DYNEELAX® and GNRB®. These tools provide essential objective data for monitoring recovery and guiding rehabilitation.

Key studies supporting the use of robotic arthrometers in rehabilitation include:
- 2016, Semay et al. (12): Demonstrated the usefulness of the GNRB in monitoring anteroposteriorlaxity after surgery, aiding in tailoring rehabilitation plans.
- 2017, Nouveau et al.(14): Highlighted the significance of understanding changes in graft compliance over time for effective rehabilitation management.
- 2023, Forelli et al.(15): Emphasized integrating arthrometer assessments into rehabilitation programs for a safer return to activities.
- 2019, Pouderoux et al.(13): Analyzed the evolution of joint laxity and graft compliance post-ACL surgery, suggesting the importance of stabilizing these factors before returning to high-impact sports.
Conclusion
In managing ACL injuries in basketball, the emphasis on prevention, early and accurate diagnosis, and personalized rehabilitation emerges as paramount. The integration of advanced diagnostic tools like the DYNEELAX® and GNRB® arthrometers into the care protocol significantly enhances the outcomes for athletes, enabling a detailed assessment of knee stability and facilitating timely interventions.
Preventive measures, including neuromuscular training (NMT) and biomechanically informed approaches, have proven effective in reducing the risk of ACL injuries. These strategies, underscored by studies, emphasize the modification of landing techniques, strengthening of the musculature around the knee, and the improvement of cognitive strategies to manage dynamic sports tasks effectively.
The role of early and accurate diagnosis cannot be overstated, with tools like the DYNEELAX® and GNRB® arthrometers providing invaluable insights into the knee’s biomechanical status. These insights are crucial for developing a targeted, personalized rehabilitation plan that addresses the specific needs and recovery trajectory of each athlete. The success of rehabilitation and the decision to return to sport are significantly enhanced by these advanced diagnostic capabilities, underscoring their importance in the standard care protocol.
In conclusion, the integration of comprehensive prevention strategies, coupled with the advancements in diagnostic and rehabilitation technologies, presents a holistic approach to ACL injury management in basketball. This approach not only mitigates the risk of initial and subsequent injuries but also supports a safer and more effective return to play, ultimately safeguarding the athletes’ careers and well-being.
Medical References (Link In DOI)
- Ryu, S. M., Na, H. D., & Shon, O. J. (2018). Diagnostic Tools for Acute Anterior Cruciate Ligament Injury: GNRB, Lachman Test, and Telos. Knee Surgery & Related Research, 30(2), 121-127. DOI: 10.5792/ksrr.17.014
- Stojanović, E., Faude, O., Nikić, M., Scanlan, A. T., Radovanović, D., & Jakovljević, V. (2023). The incidence rate of ACL injuries and ankle sprains in basketball players: A systematic review and meta-analysis. Scandinavian Journal of Medicine & Science in Sports, 33(6), 790-813. DOI: 10.1111/sms.14328
- Gill, V. S., Tummala, S. V., Boddu, S. P., Brinkman, J. C., McQuivey, K. S., & Chhabra, A. (2023). Biomechanics and situational patterns associated with anterior cruciate ligament injuries in the National Basketball Association (NBA). British Journal of Sports Medicine, 57(21), 1395-1399. DOI: 10.1136/bjsports-2023-107075
- Krosshaug, T., Nakamae, A., Boden, B. P., Engebretsen, L., Smith, G., Slauterbeck, J. R., Hewett, T. E., & Bahr, R. (2007). Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. The American Journal of Sports Medicine, 35(3), 359-367. DOI: 10.1177/0363546506293899
- Omi, Y., Sugimoto, D., Kuriyama, S., Kurihara, T., Miyamoto, K., Yun, S., Kawashima, T., & Hirose, N. (2018). Effect of Hip-Focused Injury Prevention Training for Anterior Cruciate Ligament Injury Reduction in Female Basketball Players: A 12-Year Prospective Intervention Study. The American Journal of Sports Medicine, 46(4), 852-861. DOI: 10.1177/0363546517749474
- DeFroda, S. F., Patel, D. D., Milner, J., Yang, D. S., & Owens, B. D. (2021). Performance After Anterior Cruciate Ligament Reconstruction in National Basketball Association Players. Orthopaedic Journal of Sports Medicine, 9(2), 2325967120981649. DOI: 10.1177/2325967120981649
- Tramer, J. S., Khalil, L. S., Ziedas, A., Mehran, N., & Okoroha, K. R. (2020). Return to Play and Performance in the Women’s National Basketball Association After Anterior Cruciate Ligament Reconstruction. Orthopaedic Journal of Sports Medicine, 8(9), 2325967120947078. DOI: 10.1177/2325967120947078
- Cojean T, Batailler C, Robert H, Cheze L. (2023). GNRB® laximeter with magnetic resonance imaging in clinical practice for complete and partial anterior cruciate ligament tears detection: A prospective diagnostic study with arthroscopic validation on 214 patients. Knee, 42, 373-381. DOI: 10.1016/j.knee.2023.03.017
- Magdić M, Gošnak Dahmane R, Vauhnik R. (2023). Intra-rater reliability of the knee arthrometer GNRB® for measuring knee anterior laxity in healthy active subjects. Journal of Orthopaedics. DOI: 10.1016/j.jor.2023.03.016
- Smith K, Miller N, Laslovich S. (2022). The Reliability of the GNRB® Knee Arthrometer in Measuring ACL Stiffness and Laxity: Implications for Clinical Use and Clinical Trial Design. Int J Sports Phys Ther, 17(6), 1016-1025. DOI: 10.26603/001c.38252
- Cojean, T., Batailler, C., Robert, H., Cheze, L. (2023). Sensitivity repeatability and reproducibility study with a leg prototype of a recently developed knee arthrometer: The DYNEELAX®. Medicine in Novel Technology and Devices, 19, 100254. DOI: 10.1016/j.medntd.2023.100254
- Semay, B., Rambaud, A., Philippot, R., Edouard, P. (2016). Evolution of the anteroposterior laxity by GnRB at 6 9 and 12 months post-surgical anterior cruciate ligament reconstruction. DOI: 10.1016/j.rehab.2016.07.045
- Pouderoux, T., Muller, B., Robert, H. (2019). Joint laxity and graft compliance increase during the first year following ACL reconstruction with short hamstring tendon grafts.. DOI: 10.1007/s00167-019-05711-z
- Nouveau, S., Robert, H., Viel, T. (2017). ACL Grafts Compliance During Time: Influence of Early Solicitations on the Final Stiffness of the Graft after Surgery. Journal of Orthopedic Research and Physiotherapy, 3(1), 035. DOI: 10.24966/ORP-2052/100035
- Forelli F, Le Coroller N, Gaspar M, et al. (2023). Ecological and Specific Evidence-Based Safe Return To Play After Anterior Cruciate Ligament Reconstruction In Soccer Players: A New International Paradigm. IJSPT. Published online April 2, 2023. DOI: 10.26603/001c.73031
- Leppänen, M., Pasanen, K., Kujala, U. M., Vasankari, T., Kannus, P., Äyrämö, S., Krosshaug, T., Bahr, R., Avela, J., Perttunen, J., & Parkkari, J. (2017). Stiff Landings Are Associated With Increased ACL Injury Risk in Young Female Basketball and Floorball Players. The American Journal of Sports Medicine, 45(2), 386-393. DOI: 10.1177/0363546516665810
- Waters, E. (2012). Suggestions from the field for return to sports participation following anterior cruciate ligament reconstruction: basketball. Journal of Orthopaedic & Sports Physical Therapy, 42(4), 326-336. DOI: 10.2519/jospt.2012.4005
- Taylor, J. B., Ford, K. R., Schmitz, R. J., Ross, S. E., Ackerman, T. A., & Shultz, S. J. (2018). Sport-specific biomechanical responses to an ACL injury prevention programme: A randomised controlled trial. Journal of Sports Sciences, 36(21), 2492-2501. DOI: 10.1080/02640414.2018.1465723
- Weir, G., Alderson, J., & Smailes, N. (2022). Anterior cruciate ligament injury prevention in sport: biomechanically informed approaches. Journal of Sports Sciences, 40(1), 5-15. DOI: 10.1080/02640414.2021.2018755
- Omi, Y., Sugimoto, D., Kuriyama, S., Kurihara, T., Miyamoto, K., Yun, S., Kawashima, T., & Hirose, N. (2018). Effect of Hip-Focused Injury Prevention Training for Anterior Cruciate Ligament Injury Reduction in Female Basketball Players: A 12-Year Prospective Intervention Study. The American Journal of Sports Medicine, 46(4), 852-861. DOI: 10.1177/0363546517749474
- Sugimoto, D., Myer, G. D., Barber Foss, K. D., Pepin, M. J., Micheli, L. J., & Hewett, T. E. (2016). Critical components of neuromuscular training to reduce ACL injury risk in female athletes: meta-regression analysis. British Journal of Sports Medicine, 50(20), 1259-1266. DOI: 10.1136/bjsports-2015-095596
- Klouche S, Lefevre N, Cascua S, Herman S, Gerometta A, Bohu Y. (2015). Diagnostic value of the GNRB® in relation to pressure load for complete ACL tears: A prospective case-control study of 118 subjects. Orthopaedics & Traumatology: Surgery & Research, 101(3), 297–300. DOI: 10.1016/j.otsr.2015.01.008
- Jenny J-Y, Puliero B, Schockmel G, Harnoist S, Clavert P. (2017). Experimental validation of the GNRB® for measuring anterior tibial translation. Orthopaedics & Traumatology: Surgery & Research. Received: 7 October 2016, Accepted: 30 December 2016 DOI: 10.1016/j.otsr.2016.12.011
- Mouton, C., Seil, R., Meyer, T., Agostinis, H., Theisen, D. (2015). Combined anterior and rotational laxity measurements allow characterizing personal knee laxity profiles in healthy individuals. Knee Surgery, Sports Traumatology, Arthroscopy, 23, 3571-3577. DOI: 10.1007/s00167-014-3244-6.
- Mouton, C., Theisen, D., Meyer, T., Agostinis, H., Nührenbörger, C., Pape, D., Seil, R. (2015). Combined anterior and rotational knee laxity measurements improve the diagnosis of anterior cruciate ligament injuries. Knee Surgery, Sports Traumatology, Arthroscopy, 23, 2859-2867. DOI: 10.1007/s00167-015-3757-7
- Ruiz, N., Filippi, G.J., Gagnière, B., Bowen, M., Robert, H.E. (2016). The Comparative Role of the Anterior Cruciate Ligament and Anterolateral Structures in Controlling Passive Internal Rotation of the Knee: A Biomechanical Study. DOI: 10.1016/j.arthro.2016.02.017
- Senioris, A., Rousseau, T., L’Hermette, M., Gouzy, S., Duparc, F., Dujardin, F. (2017). Validity of rotational laxity coupled with anterior translation of the knee: A cadaveric study comparing radiostereometry and the Rotab®. DOI: 10.1016/j.knee.2017.01.009