Introduction
Anterior Cruciate Ligament Injuries, or ACL injuries, are a significant concern in the field of sports medicine and orthopedics. They represent a common yet serious injury affecting the knee joint, often encountered in both athletic and general populations. The ACL, a key ligament within the knee, is essential for maintaining joint stability and enabling dynamic movements. Injuries to this ligament can lead to prolonged disability, a potential for recurrent instability, and an increased risk of degenerative joint diseases like osteoarthritis.

The proper diagnosis and management of ACL injuries are critical for optimal patient outcomes. With advances in medical technology and surgical techniques, the approach to treating these injuries has evolved, offering improved recovery and rehabilitation prospects. Furthermore, the role of sophisticated diagnostic tools, such as knee arthrometers, in accurately assessing the extent of injury cannot be overstated. These devices, including the GNRB® and DYNEELAX®, provide precise measurements of knee laxity, crucial for both diagnosis and post-treatment evaluation.
In this article, we will explore the various aspects of ACL injuries, from their pathophysiology and diagnosis to the latest treatment modalities. Our focus will extend beyond traditional methods, highlighting the significance of advanced diagnostic tools in enhancing patient care. For medical professionals striving to offer state-of-the-art care, understanding the nuances of ACL injuries and the capabilities of modern diagnostic equipment is indispensable.
1. Pathophysiology of ACL Injuries
Anterior Cruciate Ligament (ACL) injuries represent a complex interplay of anatomical, biomechanical, and physiological factors. The ACL, located within the knee joint, plays a crucial role in maintaining the joint’s stability, especially during dynamic activities involving pivoting, jumping, or sudden changes in direction. Understanding the pathophysiology of ACL injuries is essential for accurate diagnosis, effective treatment, and prevention strategies.
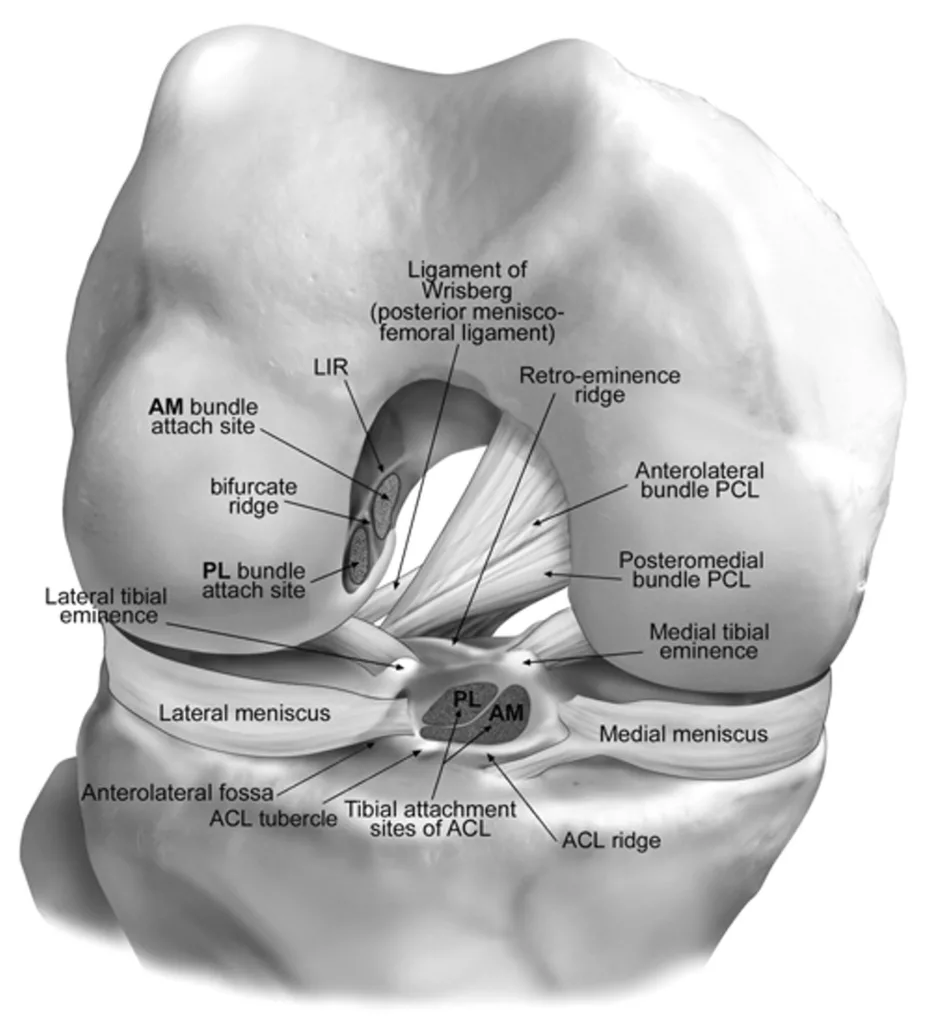
Anatomically, the ACL is one of the four major ligaments in the knee, connecting the femur to the tibia. It is composed of two bundles – the anteromedial (AM Bundle) and the posterolateral (PM Bundle), each contributing to knee stability at different angles of flexion. The ACL prevents excessive forward movement of the tibia relative to the femur and stabilizes the knee in rotational movements.
Biomechanically, ACL injuries typically occur through two primary mechanisms: contact and non-contact. Contact injuries often result from a direct blow to the knee, common in sports like football or rugby. However, non-contact injuries are more prevalent and occur due to a sudden deceleration, hyperextension, or abrupt change in direction. This mechanism is frequently seen in sports such as basketball, soccer, and skiing. In non-contact scenarios, the combination of knee valgus and internal tibial rotation is particularly detrimental, placing excessive strain on the ACL.
Hormonal influences also play a role in the susceptibility to ACL injuries, particularly in female athletes. Research indicates that fluctuations in estrogen and relaxin may affect ligament laxity and strength, potentially increasing injury risk.
The cellular response to an ACL injury involves inflammation, leading to pain and swelling. This acute inflammatory response is a double-edged sword; while it is necessary for initiating healing, excessive inflammation can lead to further damage and complications like arthrofibrosis.
Post-injury, the absence or dysfunction of the ACL leads to a biomechanically compromised knee joint. This predisposes individuals to secondary injuries, such as meniscal tears, and may accelerate the development of osteoarthritis.
In summary, ACL injuries result from a multifaceted interplay of anatomical structure, biomechanical forces, and physiological responses. Understanding these aspects is fundamental for medical professionals in diagnosing, treating, and preventing these prevalent yet impactful injuries.
2. Diagnosis and Evaluation of ACL Injuries
The diagnosis and evaluation of Anterior Cruciate Ligament (ACL) injuries require a multifaceted approach, integrating clinical assessment, imaging techniques, and advanced diagnostic tools like knee arthrometers. This comprehensive process ensures accurate diagnosis, which is crucial for effective treatment and optimal patient outcomes.
2.1 Physical Assessments

The diagnosis of ACL injuries begins with a detailed clinical examination, which is pivotal in understanding the injury’s nature and severity. The patient’s history is thoroughly reviewed, with a focus on the mechanism of injury — such as a sudden stop, pivot, or direct impact — which often provides critical clues. The physical examination is comprehensive, looking for signs of knee instability, swelling, and range of motion. Key tests include the Lachman test, which assesses anterior tibial translation and is highly sensitive for ACL tears; the anterior drawer test, which evaluates anterior displacement of the tibia; and the pivot-shift test, which can indicate rotational instability. Each test has its own sensitivity and specificity, contributing uniquely to the overall assessment of ACL integrity.
2.2 Imaging Techniques
Imaging plays an indispensable role in the confirmation of ACL injuries and the evaluation of any concomitant knee injuries. Magnetic Resonance Imaging (MRI) is the gold standard due to its ability to provide detailed visualization of the soft tissues around the knee, including the ACL, menisci, and other ligaments. MRI is highly sensitive and specific for ACL tears and is invaluable in detecting subtle injuries and planning surgical interventions. Additionally, it aids in identifying associated injuries such as meniscal tears or damage to collateral ligaments, which are crucial for comprehensive treatment planning. The clarity and detail offered by MRI images facilitate a more accurate diagnosis, enabling tailored treatment strategies that address all aspects of the knee injury.
2.3 Advanced Diagnostic Tools: Arthrometers
The introduction of knee arthrometers, such as the GNRB® and DYNEELAX®, has revolutionized the assessment of knee laxity and stability. These tools provide quantitative data on knee laxity, which is particularly beneficial in ambiguous cases or for postoperative evaluation. Studies like Klouche et al. (2015) highlight the diagnostic value of the GNRB in relation to pressure load for complete ACL tears, showcasing its efficacy in clinical settings. The GNRB system was also specifically evaluated for its efficacy in assessing knee laxity in studies like Robert et al. (2009).
Innovative Rotation Analysis: Recent advancements in knee arthrometry, including the analysis of rotational laxity, bring a new dimension to ACL injury evaluation. This approach allows for a more comprehensive assessment of the knee, considering both anterior-posterior and rotational stability. Mouton et al. (2014) emphasized the importance of combined anterior and rotational laxity measurements, which can characterize individual knee laxity profiles, providing invaluable information for personalized treatment strategies. Additionally, Jenny et al. (2017) validated the GNRB for measuring anterior tibial translation, demonstrating its accuracy and reliability in comparison with standard navigation systems.
Comparative Studies: Recent research, such as the study by Cojean et al. (2023), compares the effectiveness of MRI and the GNRB in ACL injury diagnosis, offering insights into the practical applications and advantages of these diagnostic tools in various clinical scenarios.

In summary, the diagnosis and evaluation of ACL injuries involve a combination of physical assessments, imaging, and the use of advanced tools like knee arthrometers. Incorporating innovative techniques such as rotation analysis and considering findings from recent studies ensures a comprehensive and accurate diagnosis, forming the basis for effective treatment planning.
3. Treatment Modalities for ACL Injuries
3.1 Conservative Management
Non-surgical treatment options for ACL injuries are typically considered for patients with low activity levels or specific clinical scenarios. These include physical therapy, bracing, and lifestyle modifications. Physical therapy focuses on strengthening the muscles around the knee, improving stability, and restoring range of motion. Conservative management is often indicated for partial tears or in patients where surgery poses higher risks.
3.2 Surgical Intervention

ACL reconstruction surgery is the standard treatment for active individuals suffuring from complete tears. Various surgical techniques exist, involving the replacement of the torn ligament with a graft. Common graft sources include the patient’s own patellar tendon, hamstring tendon, or a donor tissue (allograft). The choice of technique and graft depends on individual factors like age, activity level, and specific knee characteristics. Autografts (from the patient) generally have quicker integration but require additional incisions, whereas allografts (donor tissue) reduce surgery time but may have slower integration.
3.3 Postoperative Rehabilitation
Rehabilitation following ACL surgery is critical, and incorporating arthrometer measurements can significantly enhance its effectiveness. Studies like Semay et al. (2016) demonstrate the value of using devices like the GNRB to monitor anteroposterior laxity post-surgery, providing objective data crucial for tailoring rehabilitation and determining readiness for return to sports. Nouveau et al. (2017) further highlight the importance of understanding graft compliance over time, where early solicitations on the graft can influence its final stiffness post-surgery, underscoring the role of precise measurement tools in managing rehabilitation. Forelli et al. (2023) emphasize the integration of such assessments into a comprehensive rehabilitation program, ensuring a safer and more effective return to activity. These studies collectively underscore the importance of using arthrometers like the GNRB® and DYNEELAX® in postoperative rehabilitation to guide decision-making and optimize patient outcomes.
4. Innovations in ACL Injury Management
4.1 Emerging Techniques
New surgical techniques and treatment modalities in ACL injury management are making significant strides. Minimally invasive arthroscopic procedures are reducing recovery times and scarring. Advances in regenerative medicine, such as stem cell (Mario Hevesi et al. 2019; DOI: 10.1007/s12178-019-09580-4) and PRP therapies (Ting Zhu et al., 2022; DOI: 10.1177/23259671211061535), are exploring enhanced ligament healing. Biomechanical research is improving surgical techniques for more accurate ACL reconstructions. Notably, the Bridge-Enhanced ACL Repair (BEAR) technique is gaining attention as an innovative approach (Martha M. Murray et al., 2016; DOI: 10.1177/2325967116672176), focusing on stimulating natural ligament healing without the need for traditional grafts.
4.2 Advanced Diagnostic Tools Revisited
The importance of advanced diagnostic tools, such as the GNRB® and DYNEELAX®, in ACL injury management cannot be overstated. These sophisticated devices offer precise and objective measurements of knee laxity: translational and rotational stability, which are crucial in both diagnosing ACL injuries and evaluating the effectiveness of surgical reconstructions. Unlike MRI analysis, which assesses the knee in a static state, arthrometers recreate real-life conditions, providing dynamic insights. This complements MRI’s static analysis, offering a more comprehensive view. By providing detailed insights into knee biomechanics, these tools enable clinicians to tailor treatment plans more accurately to individual patient needs. This approach represents a significant shift towards personalized and data-driven care in orthopedics, ensuring optimal outcomes for patients with ACL injuries.
Conclusion
In summary, the management of Anterior Cruciate Ligament (ACL) injuries involves a comprehensive approach encompassing diagnosis, treatment, and rehabilitation. Advanced diagnostic tools like the GNRB® and DYNEELAX® have revolutionized the evaluation process, offering precise, dynamic assessments that complement traditional methods like MRI. Surgical techniques, including minimally invasive procedures and the promising BEAR technique, continue to evolve, enhancing patient outcomes.
Looking ahead, the future of ACL injury management is poised for further advancements, particularly in personalized treatment and regenerative medicine. The integration of innovative diagnostic tools and surgical methods will continue to refine our approach to these injuries.
Staying abreast of the latest tools and techniques is crucial for practitioners in this field. Products like the GNRB & Dyneelax represent the forefront of this evolution, offering opportunities to enhance patient care and outcomes significantly.
Medical References
- Robert, H. et al. (2009). GNRB Study on Knee Laxity Evaluation. Orthopedic Surgery and Research. DOI: 10.1016/j.otsr.2009.03.009
- Jenny, J.Y. et al. (2013). Anterior Knee Laxity Measurement using Stress Radiographs and the GNRB System vs. Intraoperative Navigation. Orthopaedics & Traumatology: Surgery & Research. DOI: 10.1016/j.otsr.2013.07.008
- Mouton, C. et al. (2014). Personal Knee Laxity Profiles in Healthy Individuals: Combined Anterior and Rotational Laxity Measurements. Journal of Biomechanics. DOI: 10.1007/s00167-014-3244-6
- Klouche, S. et al. (2015). Diagnostic Value of the GNRB for Complete ACL Tears. Orthopaedics & Traumatology: Surgery & Research. DOI: 10.1016/j.otsr.2015.01.008
- Jenny, J.Y. et al. (2017). Experimental Validation of the GNRB for Measuring Anterior Tibial Translation. Journal of Knee Surgery. DOI: 10.1016/j.otsr.2016.12.011
- Cojean, T. (2023). MRI vs. GNRB in ACL Injuries Detection: A Comparative Study. Journal of Orthopedic Research and Therapy. DOI: 10.1016/j.knee.2023.03.017
- Cojean, T. (2023). Sensitivity, Repeatability, and Reproducibility Study with a Leg Prototype of a Recently Developed Knee Arthrometer Dyneelax. Journal of Biomechanics. DOI: 10.1016/j.medntd.2023.100254
- Smith, K. (2022). The Reliability of the GNRB Knee Arthrometer in Measuring ACL Stiffness and Laxity: Implications for Clinical Use and Trial Design. Journal of Orthopedic Research and Therapy. DOI: 10.26603/001c.38252
- Semay, B. et al. (2016). Evolution of Anteroposterior Laxity by GNRB at 6, 9, and 12 Months Post-Surgical ACL Reconstruction. Journal of Knee Surgery. DOI: 10.1016/j.rehab.2016.07.045
- Robert, Nouveau et al. (2017). ACL Grafts Compliance: Influence of Early Solicitations on Final Stiffness Post-Surgery. Journal of Orthopedic Research and Therapy. DOI: 10.24966/ORP-2052/100035
- Forelli, G. (2023). After Surgery Rehab Post-Op. Journal of Rehabilitation Medicine. DOI: 10.26603/001c.73031
- Murray, M.M. et al. (2016). The Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR) Procedure: An Early Feasibility Cohort Study. Orthopaedic Journal of Sports Medicine. DOI: 10.1177/2325967116672176.
- Hevesi, M. et al. (2019). Stem Cell Treatment for Ligament Repair and Reconstruction. Current Reviews in Musculoskeletal Medicine. DOI: 10.1007/s12178-019-09580-4.
- Zhu, T. et al. (2022). Effects of Platelet-Rich Plasma on Clinical Outcomes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis. Orthopaedic Journal of Sports Medicine. DOI: 10.1177/23259671211061535.